Learning the distinction between anencephaly and acrania is important to expectant mothers and medical experts. Both disorders are serious neural tube defects (NTDs) that interfere with fetus development, yet they are different in terms of the formation of the brain and skull. Acrania happens when the skull defect exposes the brain tissue whereas anencephaly is characterized by loss of brain structure. Early detection of these complications with prenatal diagnosis such as ultrasound or mother serum alpha-fetoprotein screening assist the family to make a well-informed choice. This article examines their causes, risk factors and prognosis and prevention measures and provides evidence-based concise, clear information that provides the reader with the power to comprehend and prepare to such problematic conditions.
Introduction about Neural Tube Defects
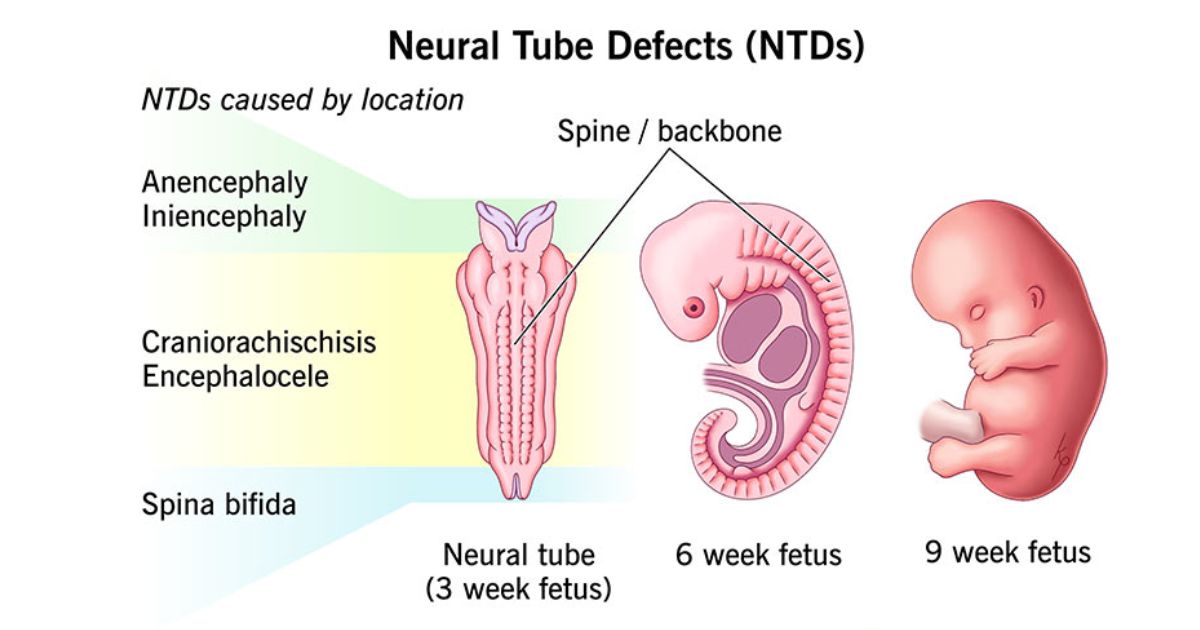
Any parent would wish to have a healthy infant but there are occasions when neural tube defects (NTDs) interfere with the normal pregnancy. These birth defects occur at a very very early stage of fetus growth, normally at the first month of conception. The CDC indicates that NTDs such as spina bifida, acrania, and anencephaly affect almost 3,000 pregnancies annually in the U.S. Learning them is not merely medical interest, but will assist families with the emotional preparation, find adequate care and make informed decisions regarding their pregnancy. Women may also be empowered through early education to prevent before conception.
What is Acrania?
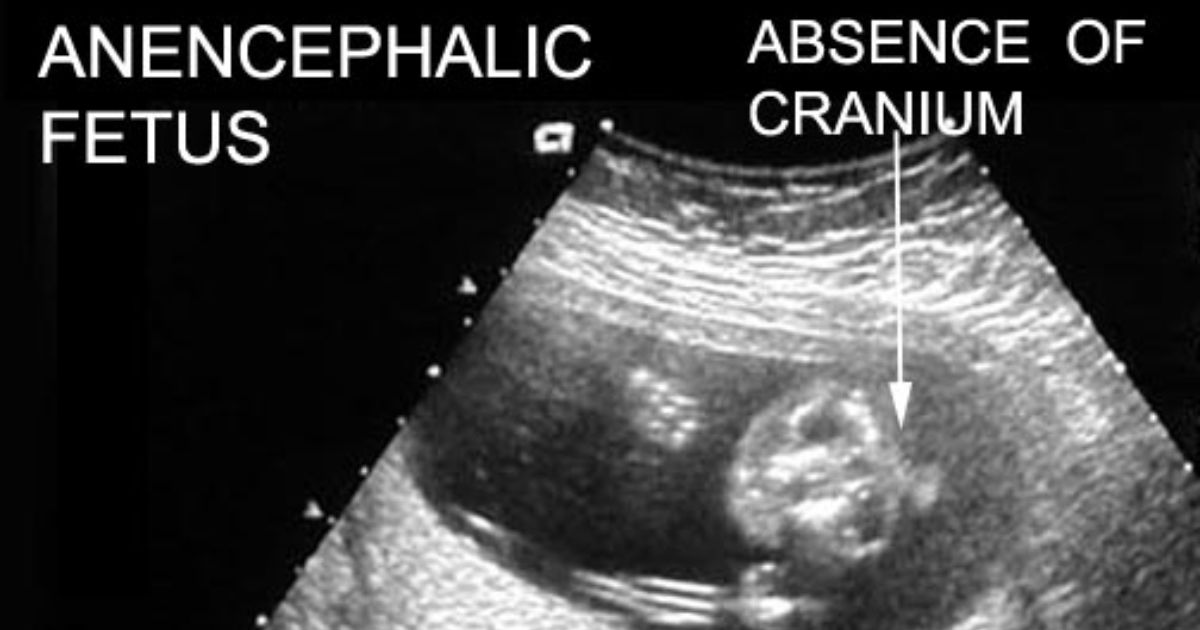
The answer to the question of what is acrania can be devastating when asked by people. Acrania is a severe and rare disorder in which the skull bones of the baby do not develop and the brain tissue is exposed and not covered. It is among the initial neural tube defects which may be detected during the first trimester in acrania diagnosis by ultrasound imaging as early as 11 weeks. The brain develops normally without the skull to cover it but over time, with the continuation of pregnancy, it may gradually degenerate. Cases have been published of babies born alive with acrania but surviving only minutes or hours, just how life-threatening skull formation is outside the womb.
What is Anencephaly?
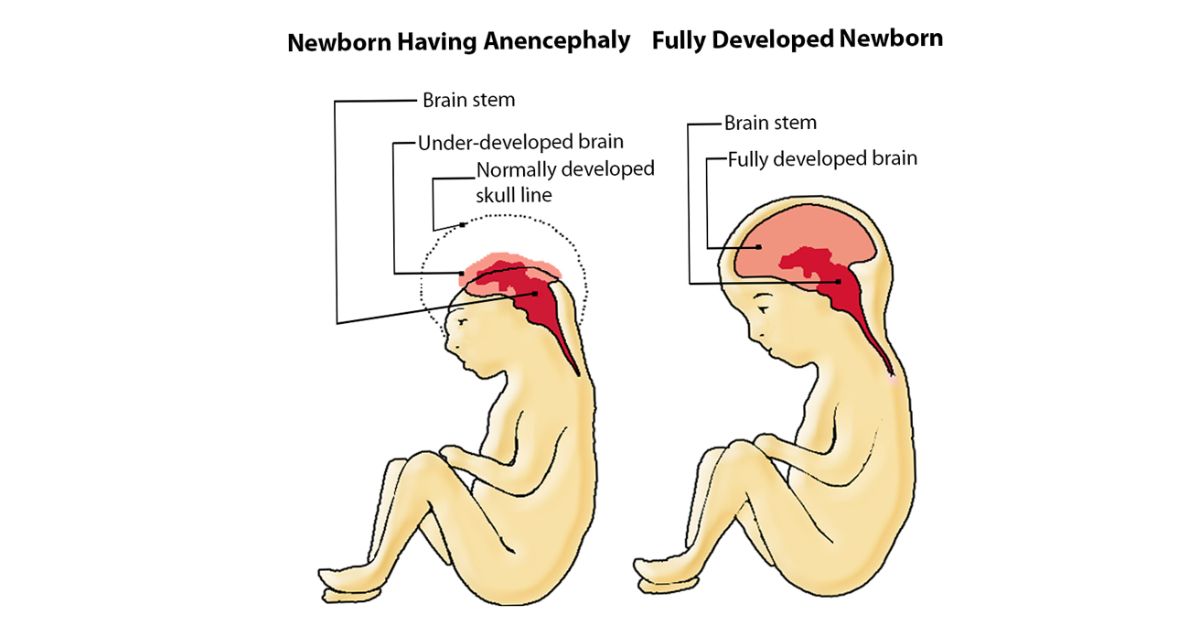
One of the questions that people tend to ask is what is anencephaly and what is the difference between anencephaly and acrania. Anencephaly is said to be a more severe anomaly, in which the brain and skull fail to develop and a majority of the brain tissue is absent. The disorder is nearly always lethal and the vast majority of the infants concerned pass away before or shortly after birth.
The current rate of anencephaly in the U.S is about 1 in 4,600 babies, according to the March of Dimes. There are also cases of earlier termination of the pregnancy by miscarriage or stillbirth, in which case the less number of affected conceptions could be greater. Since this is such a devastating diagnosis, families would tend to refer to a specialist in maternal-fetal medicine and consult with them immediately to get counseling.
Major Differences between Acrania and Anencephaly
The two conditions do not differ even though they are related. Acrania is an imperfection of the skull whereby the brain is still intact but exposed whereas anencephaly is a serious brain destruction and almost total lack of the cranial vault. An example that is useful in clarifying the distinction between acrania and anencephaly is the following:
| Findings | Acrania | Anencephaly |
| Skull Presence | Absence of skull bones | Skull missing, brain tissue atrophied. |
| Brain Tissue | Current but uncovered | Mostly not present. |
| Detection | First trimester early | Later on in the pregnancy. |
| Prognosis | Death without treatment | 50% mortality of stillbirth. |
| Outcome | Outcome May develop into anencephaly | Fatally before or after birth. |
This table explains why acrania is in some cases referred to as the precursor lesion of anencephaly. There is early detection of acrania so that the parents know how it is likely to proceed and are ready about what to expect in future.
Etiology and Risk Factor of Acrania and Anencephaly
To figure out the reasons behind the development of these conditions, it is necessary to examine a number of biological and lifestyle factors. Neural tube defects have both a genetic basis and an environmental one, so their prevention is not easily achievable still.
Genetic Predisposition
Families are more likely to have NTDs because of the variants of genes that influence the metabolism of folate. This refers to genetic predisposition, which implies that despite the nutritional adequacy, the risk can be high. Genetic counseling may be used to determine this risk and preconceptional care.
Nutritional Deficiency
Poor folate is one of the greatest contributors. A deficiency in folic acid supplementation during early pregnancy and before the pregnancy is risky. This is the reason why governments are urging women to consume fortified diets, and use daily supplements.
Maternal Health Conditions
Obesity and maternal diabetes have been attributed to increased NTD. The early pregnancy may disrupt the normal development of the fetus because of the uncontrolled sugar levels in the blood. One of the triggers also includes high fever or hyperthermia during the first trimester.
Drug and Environmental Interference
Some anti-seizure medications, particularly, valproic acid, may contribute to the development of NTD. The role of exposure to dangerous chemicals or radiations during early pregnancy may also be of importance, which is why special attention should be paid to prenatal care.
Recurrence Risk
Women that have experienced a single pregnancy of acrania or anencephaly are prone to 2-5 percent recurrence in subsequent pregnancies. This renders preconception planning and early surveillance important in taking risks out of the later pregnancies.
Fetal Development: How Acacia causes Anencephaly?
In the early development of the fetus, the skull and the brain develop as a very coordinated process. In case of the violation of this process, such conditions as acrania and anencephaly may arise. This chronological developmental process can make the parents and doctors appreciate the importance of early detection.
- The neural tube is sealed by day 28 of gestation, and when it fails at the cranial end, there is acrania.
- The skull vault is missing in acrania; the developing brain is not covered by the amniotic fluid.
- The long-term effects include exposure through which the brain herniates and degenerates.
- This degeneration causes acrania to change into exencephaly (brain protrusion) and finally anencephaly.
- The research shows that out of the pregnancies on which acrania is identified beyond the first trimester, more than 95% of them develop anencephaly.
- Acrania can be detected through early ultrasound imaging as early as 11 weeks so that parents and clinicians can discuss management.
- Research indicates that maternal-fetal medicine experts focus on early detection since it will enable them to make informed decisions and plans.
- Early detection of acrania can be used to assist with prenatal diagnosis of similar conditions like encephalocele or microcephaly.
Symptoms and Signs in Pregnancy
Even severe neural tube defects (NTDs) such as acrania or anencephaly may still make the pregnancy feel normal. Since these conditions have no physical manifestations in most cases, medical screening is very essential in revealing them during pregnancies.
- Majority of pregnant women do not show any external symptoms and therefore normal prenatal testing is the initial indicator that something could go amiss.
- High maternal blood AFP levels tend to show that the neural tube is open.
- When the levels of AFP are not normal, specific ultrasound scans are done to check on the defects of the skull or on whether the brain has exposed tissue.
- Brain herniation or cranial bone deficiency is observable in the first trimester using high-resolution ultrasound.
- In case of unclear ultrasound results, fetal MRI can be suggested to rule out the diagnosis and exclude other conditions like microcephaly or encephalocele.
- Some pregnancies also reveal to have excess amniotic fluid (polyhydramnios), which is also a suspicion to NTDs.
- Early diagnosis enables the doctor to address the parents on prognosis and pregnancy, assisting them make the right choices.
Prenatal Diagnosis and Prenatal Screening
The early diagnosis of acrania or anencephaly is important since majority of mothers have no warning signs. Early screening provides the healthcare providers with the opportunity to respond swiftly and deliver optimal care and counseling to the families.

- Maternal serum alpha-fetoprotein (AFP): The level of alpha-fetoprotein in the serum of the mother is often high in case the neural tube is open, so it is an important initial screening test.
- In case of abnormal AFP test, physicians conduct an in-depth ultrasound imaging to ensure there are no skull bones or apparent brain herniation.
- The first trimester ultrasound may often identify acrania at 1114 weeks, which aids in decision making early.
- In more complicated situations, fetal MRI is applied to verify the results as well as assess the possibility of such related conditions as microcephaly or encephalocele.
- Amniocentesis can be proposed in case of a suspicion that the genetic syndromes can happen, allowing to perform chromosomal analysis, as well as to detect any other potential risk factors.
- Other effects include early diagnosis that can be used to estimate the risk of recurrence and future pregnancy planning with the assistance of the maternal-fetal medicine specialist.
Pregnancy Outcomes and Prognosis
Medical advances have a very low prognosis as far as babies with acrania or anencephaly are concerned. Such conditions have been determined as being incompatible with long-term survival as vital brain parts fail to develop or are increasingly destroyed.
Pregnancy Outcomes
The majority of affected pregnancies with acrania or anencephaly lead to miscarriage or still birth i.e. before 20-24 gestation weeks. The CDC statistics indicate that anencephaly occurs in approximately 3 out of 10,000 pregnancies in the US and most of them spontaneously miscarry.
Survival After Birth
Even in the limited instances that the baby is carried to term, it survives in minutes to a few hours. There have been some case studies of survival of up to 2-3 days but no reported long-term survival. Such infants normally do not have the brain structures that sustain life, control breathing and the ability to be conscious.
Planning and Support
The awareness of the probable result allows families to make decisions that are based on their desires and beliefs. Parents can decide to have a delivery at a place where they can have immediate access to the skin to skin contact, take photos and create memories. Mothers and palliative care teams can facilitate the organization of the loving birth plan.
Prevention: Folic Academic and Maternal Care
Folic acid supplementation before pregnancy and in early stages of pregnancy is the best preventive strategy. The CDC suggests 400 mcg every day to any woman of child-bearing age. Research indicates that following grains fortification with folic acid in the U.S, the number of NTDs decreased by approximately 35%. Risk can further be reduced by taking care of good health, managing diabetes, and not taking damaging drugs in early pregnancy or overheating the unborn baby.
Significance of Folic Acid in Prevention
Sufficient folate consumption is one of the most efficient mechanisms of preventing acrania and anencephaly as neural tube defects (NTDs). Evidence indicates that women who conceive at least one month with folic acid supplements and in the first quarter of pregnancy can lower their chances of getting NTDs by up to 70. Mandatory fortification of fortified food, including cereals and grains, has also greatly reduced the occurrence of NTDs in the U.S., as the law has been enacted since the year 1998.
Maternal Care and Lifestyle
In-depth maternal care is equally significant. Planning women who are pregnant are advised to control long-term diseases like diabetes, take no dangerous drugs such as some anti-seizures, and have a healthy weight. It is also possible to prevent high fever during the initial pregnancy, proper nutrition, and avoidance of toxic environmental exposures to prevent risk.
Genetic Counseling and Preconception Planning
Genetic counseling of neural tube defects can be used on couples who have a history of a previous NTD-affected pregnancy. Counselors can prescribe greater doses of folic acid and prenatal diagnosis at an early age through ultrasound or maternal serum alpha-fetoprotein (AFP) to identify recurrence at an early stage. This will enable the parents to make sound judgments and get emotional support during the process.
Treatment of Acrania and Anencephaly
Parents have hard choices to make in cases of a confirmed diagnosis. It is a meeting with a team of perinatologists, neonatologists and genetic counselors to facilitate a care plan to the family. Others opt perinatal palliative care which is based on comfort and emotional bonding in the time they have. Other ones venture into termination based on state laws. Psychological support and future pregnancy information should be provided during counseling to minimize the chances of a relapse.
Prenatal Support and Counseling of the Pregnant’s
It can be devastating to be diagnosed with such a condition. The families are supposed to find professional counseling services and reach support networks. Genetic counseling of neural tube defects assists in giving parents the knowledge on recurrence risk and prevention methods of similar cases in future pregnancies. March of dimes and other local grief organizations offer a safe setting to cope with grief and have hope. The fact that we were not alone, as one parent told, assisted us in getting through one of the most difficult moments we had in our lives.
Why Early Detection Matters?
The distinction of the acrania and anencephaly is medically critical and emotionally critical. The timely identification of the neural tube defects gives parents the opportunity to make a wise decision, be prepared emotionally and safeguard the well-being of the mother. Prevention programs, educational activities, and public awareness measures would help a great deal in diminishing these tragic consequences and make sure that families are provided with the support and compassionate care.
FAQ‘s
1. How does acrania differ with anencephaly mostly?
Acrania is lack of the skull bones but the brain is intact, whereas anencephaly is the lack of or destruction of the huge portions of the brain.
2. Are the neural tube defects preventable?
Yes, most of them can be diminished by taking folic acid supplementary prior to conception and early pregnancy, as well as by giving appropriate maternal care.
3. What is the earliest time that acrania or anencephaly can be identified?
They may be identified early during the first trimester, either by using ultrasound or by high levels of maternal serum alpha-fetoprotein (AFP).
4. What happens to the pregnancy with anencephaly?
Regrettably, the survival is not good. Majority of the pregnancies end up in miscarriage and those that proceed to delivery normally last few minutes or hours.
5. Whom do I liaise with once I have been diagnosed with NTD?
You are to visit a palliative care team, a maternal-fetal medicine specialist, and a genetic counselor perhaps, to organize the management of the pregnancy and emotional support.

 Medically reviewed by
Medically reviewed by