You may have cytolytic vaginosis in case you have ever struggled with itchy vulvovaginal skin, continuous abnormal vaginal discharge, or pain during sexual intercourse without alleviation with any yeast infection medication. This is a condition also referred to as lactobacillus overgrowth syndrome that occurs when the vaginal microbiome is too acidic as a result of excess growth of good bacteria. It may lead to pain, wrong diagnosis and emotional tension. It is important to know how to cure and treat it to have a balance and confidence once again. Here we will cover and discuss all you should know about baking soda douche remedies to long-time prevention so that you can finally enjoy permanent relief.
What is Cytolytic Vaginosis?
Cytolytic vaginosis is a disease that is characterized by excess hydrogen peroxide-producing lactobacilli in the vaginal flora. In regular circumstances, the bacteria prevent the proliferation of bad microbes, but an excess of them leads to an excessively acidic environment. This destroys the vaginal epithelial cells causing symptoms that resemble the yeast infections. Research indicates that almost 5 to 7 percent of the women who experience chronic vaginal symptoms can actually have this condition yet they are never diagnosed since standard lab tests are otherwise designed to examine the yeast or bacterial vaginosis.
The causes of Cytolytic Vaginosis
Disproportion of the fragile microbiome of the vagina is the primary reason of cytolytic vaginosis. With excess growth of lactobacilli, the vaginal PH turns excessively acidic resulting in a process known as vaginal cytolysis. This leads to the destruction of vaginal epithelial cells leaving bare nuclei and cytoplasmic debris which appear on a wet smear under the microscope. The change tends to occur because of natural hormonal changes especially in the luteal phase, although external influences may aggravate the condition. Before the actual cause is discovered, many women are repeatedly misdiagnosed and treated as a result of having a yeast infection.
Typical Notions that lead to Cytolytic Vaginosis:
- Luteal changes in hormones.
- High estrogen levels
- Hormonal changes during pregnancy
- Excessive probiotic intake
- Frequent antibiotic use
- Overuse of vaginal douches
- Immunological imbalance and chronic stress
- Poorly controlled diabetes
- Non-breathable tight clothing
- There were frequent misdiagnosis with candidiasis
Risk Factors: Who is at the Highest Risk of getting it?
Cytolytic vaginosis is most common in women in their reproductive age and is especially likely to develop when their symptoms increase during the luteal period of the menstrual cycle. Glycogen is made more accessible by postnatal modifications in the vaginal flora in pregnancy or in diabetic women, which contributes to lactobacillus overgrowth syndrome. Repeated antibiotic treatment or self-medication with probiotics may further disturb the vaginal microbiome, which increases the frequency of flare-ups. When you had a history of vaginal irritation repeatedly with negative cultures, it is a condition that should surely be included in the discussion list with your medical worker.
Most Common Risk Factors:
- Reproductive age
- Changes in luteal phase hormone.
- Pregnancy
- Diabetes
- Frequent antibiotic use
- Over the counter probiotic supplementation
- High estrogen therapy
- Frequent treatment of yeast infections
- Tight, synthetic underwear
- Excessive use of vaginal cleansers
Signs of Cytolytic Vaginosis
The symptoms tend to mix with other vaginal diseases and this is the reason why misdiagnosis with candidiasis is high. Women tend to complain of whitish odourless discharge that has cottage cheese texture, but no odour of bacterial vaginosis. Vulvar erythema and vulvar oedema are frequent and lead to burning or itching of a severe nature. Common complaints are painful urination (dysuria) and painful sex (dyspareunia). These symptoms can be cycle associated, with a higher level of occurrence in the second half of the cycle, when the estrogen levels are high.
| Symptom | How It Differs from Yeast Infection |
| Whitish odourless discharge | No foul smell, unlike BV |
| Vulvovaginal itching | Often cyclical, worsens pre-period |
| Pain during sex (dyspareunia) | More from acidity than infection |
| Dysuria | Mild burning, not intense pain |
Problems and Adverse Effects on Vaginal Health
Even though cytolytic vaginosis may not be considered a harmful medical condition, its effects on the life of a woman can be significant in the long-term. Constant irritation may cause discomfort during intimacy, cause insomnia and even undermine self esteem. Most women complain of psychological effects of chronic vaginal symptoms such as anxiety, embarrassment, and fear of sexually transmitted diseases. It is always mistaken, and the vaginal microbiome is likely to be disrupted by the frequent application of antifungal creams or antibiotics, which will only prolong the issue rather than resolve it. Unattended, the condition can produce a loop of frustration that impacts the relationships and emotional wellbeing.

Typical Problems of Cytolytic Vaginosis:
- Perennial vulvovaginal itching
- Relentless white odourless drain
- Sexache (sexy pain) during sexual intercourse (dyspareunia)
- Pain on urination (dysuria)
- Vulvar erythema and oedema
- Sleep disruption
- Symptom-related anxiety and stres
- Pressure on intimate relationships
- Decreased quality of life
- Incidents of chronic candida misdiagnosis
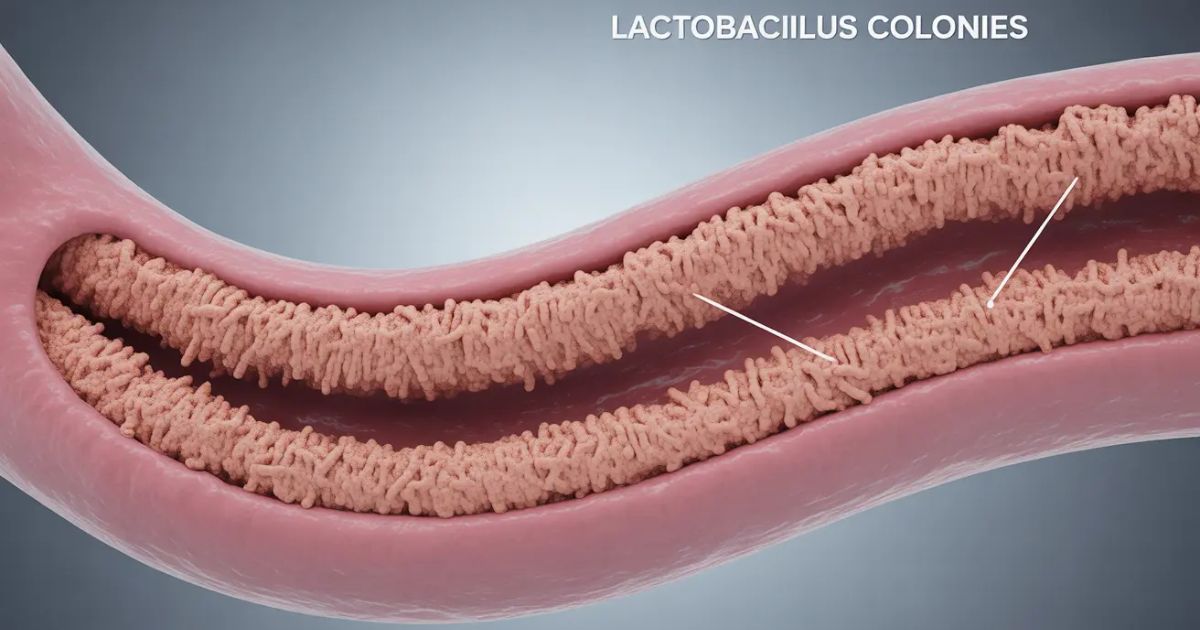
Pathogenesis: The Role of Lactobacilli in Cytolytic Vaginosis
The pathogenesis of the cytolytic vaginosis should be understood to halt the misdiagnosis cycle. Vagina has a rich vaginal microbiome, which is mostly dominated by lactobacilli that tend to keep infections away by ensuring that there is a slightly acidic environment. However, at excessive levels of proliferation, these bacteria cause an excessively acidic condition known as lactobacillus overgrowth syndrome or Doderleins cytolysis. This changes to cell destruction, irritation and whitish odourless discharge which commonly mistakes the condition to be yeast infections. Research indicates that 5-7 percent or more women experiencing chronic vaginal symptoms can actually have the condition but are wrongly diagnosed on repeated occasions.
The normal mechanism of Lactobacilli
Lactobacilli in a healthy vaginal setting secrete lactic acid, hydrogen peroxide and antimicrobial substances, which serve as natural defense mechanisms. They maintain the vaginal pH at a constant level of 3.8 to 4.5 keeping the vagina defensible to infections and in balance with the vaginal microbiome.
The Process of Overgrowth
Cases When lactobacilli that produce hydrogen peroxide overgrow, the vaginal pH becomes too low. This causes vaginal cytolysis which is the breakdown of vaginal epithelial cells. The wiped nuclei and cytoplasmic debris are observed under a microscope on a wet smear / wet mount which is a classic indication that this is not a yeast infection.
The Cause of the Disturbance of the Balance
It can change because of hormonal spikes during the luteal phase, pregnancy, estrogen treatment or even lifestyle practices such as over-taking of probiotics. Imagine that it is a garden in which one plant grows wildly, and chokes the rest of them, the ecosystem becomes deprived of its diversity, and the symptoms emerge.
Prolonged Effect on Vaginal Health
Unattended, the overly acidic condition results in chronic irritability, erythema of the vulva, edema and dyspareunia (painful sex). In the long term, that may lead to such emotional stress and sleeping issues as well as frequent failures of the treatment process, and the correct diagnosis is essential to provide relief in the long term.
Diagnosis: What Doctors How to Diagnose Cytolytic Vaginosis?
Physicians begin with a thorough symptom history, commonly inquiring when the symptoms are aggravated, most women say its exacerbations happen on the luteal phase of the menstrual cycle. Then there is a physical examination and laboratory tests. Diagnosis of cytolytic vaginosis with wet smear? A vaginal fluid showing a specific condition is collected on a slide and subjected to microscopic examination by your healthcare provider.
Microscopic Findings
They observe 3 characteristic results under the microscope; bare nuclei, cytoplasmic debris and excess of vaginal epithelial cells. Vaginal pH tends to be extremely low (3.5 4.0) and that is why, the vaginal pH cannot be mistaken with bacterial vaginosis, as the pH is generally higher than 4.5. Significantly, no clue cells (in BV) and no yeast forms (in candidiasis).

Wet Mount and Gram Stain
Physicians can also order a wet mount or Gram stain to see hydrogen peroxide-producing lactobacilli, which were present in large numbers in lactobacillus overgrowth syndrome. One of the most critical components of the diagnosis is the ruling out of other conditions, in fact, candidiasis, bacterial vaginosis, and trichomoniasis are usually categorized because otherwise, a provider is prone to misdiagnosis and prescribe antifungal or antibiotic medications that are not needed.
Additional Tests
A pH strip test and a KOH whiff test are also performed in fewer instances, and these normally have negative results regarding an infection. It is advised by many professionals to take into consideration cytolytic vaginosis where the woman has undergone yeast infection treatment and fails to receive results.
Diagnostic Table
| Test | Finding in Cytolytic Vaginosis |
| Vaginal pH | Low (3.5–4.0) |
| Microscopy | Bare nuclei, cytoplasmic debris |
| Clue cells (BV marker) | Absent |
| Yeast / hyphae | Absent |
| Lactobacilli | Overgrowth, abundant |
Relevance of Proper Diagnosis
Correct diagnosis is important since wrong diagnosis with candidiasis may result in several months of antifungal treatment, which actually increased the imbalance of the vaginal microbiome. This condition is identified early thus saving time, money and emotional strain.
Differential Diagnosis: Diseases that look like Cytolytic Vaginosis
Various states resemble cytolytic vaginosis, and that is why it is complicated to diagnosis it. Bacterial vaginosis is normally characterized by fishy odor, elevated vaginal PH and the presence of clue cells whereas CV is characterized by the absence of an odor and lower PH. Candidiasis is discharged in thick cottage cheese-like discharge and is responsive to antifungals- unlike CV. Trichomoniasis presents with frothy foul-smelling discharge and is motile under the microscope. Postmenopausal atrophic vaginitis is normally manifested by dryness as opposed to discharge.
Comparison Table: Cytolytic Vaginosis vs Other Conditions.
| Condition | pH Level | Microscopy | Odor | Key Distinguishing Feature |
| Cytolytic Vaginosis | 3.5–4.0 | Bare nuclei, cytoplasmic debris | None | Lactobacilli overgrowth, low pH |
| Bacterial Vaginosis (BV) | >4.5 | Clue cells present | Fishy (amine) odor | Thin grayish discharge, positive whiff test |
| Candidiasis (Yeast) | 4.0–4.5 | Budding yeast, hyphae | None | Thick white discharge, responds to antifungal meds |
| Trichomoniasis | >4.5 | Motile protozoa, WBCs | Foul odor | Frothy green discharge, STD-related |
| Atrophic Vaginitis | >5.0 | Few epithelial cells | None | Vaginal dryness, low estrogen state |
Treatment of Cytolytic Vaginosis
Therapy of cytolytic vaginosis is aimed at the restoration of normal vaginal pH and the decrease in the proliferation of lactobacilli. Antifungal or antibiotic therapy is not effective and can delay the symptoms of the disease unlike bacterial vaginosis or a yeast infection. I believe that the safest option is to begin with simple home treatments such as baking soda sitz baths in order to achieve an aim at restoring the vaginal environment to its normal state as smoothly as possible.
General Measures
Physicians tend to prescribe against unnecessary antifungal medicine and pH correction. To minimize irritation and promote the natural vaginal microbiome, it is possible to wear breathable cotton underwear, use harsh soaps, and omit scented products. Other effects that many women report include improvement by not using any unnecessary probiotic supplements in the process of treatment.
Specific Treatments
A baking soda douche or a sitz bath, administered multiple days under medical care, is one of the most used treatment methods to increase the vaginal pH. It is regarded as a safe method of intravaginal use of baking soda, since it soothes the vagina, and decreases the excess acidity of the vagina due to the presence of lactobacilli that produce hydrogen peroxide. Majority of the cases are cured in within a week, however in severe or recurrent cases, the treatment may take longer or repeat therapy.
Medical Follow-Up
To be sure that the number of vaginal epithelial cells and lactobacilli takes the normal level, your physician might prescribe subsequent wet smear / wet mount tests. In case the symptoms remain unchanged even under treatment, additional examination is required to exclude candidiasia, bacterial vaginosis, and other diseases.
Symptom Remedies: Lifestyle and Home-Based
Cytolytic vaginosis has several home remedies that are useful in ensuring that comfort is maintained. Loosely-fitting cotton underwear can help to minimize the amount of moisture, whereas perfumed soaps and douching can be minimized to minimize irritation. It can be of insight to your doctor to monitor your symptoms and record their occurrence during the cycle as they increase. Home-based vaginal alkalisation with baking soda sitz baths is one of the methods of relief.
Prevention: The ways of lowering your risk of cytolytic vaginosis

Cytolytic vaginosis has a large variety of safe home remedies which may be used to aid recovery and maintain the symptoms in control. These strategies pay attention to the minimization of irritation, the balance of the vaginal microbiome, and the prevention of relapses.
- Wear free cotton underwear: it will provide a reduced amount of moisture and a higher level of air circulation to eliminate additional development of lactobacilli.
- Do not use perfumed soaps or scented products: These may upset the natural vaginal pH and exacerbate vulvovaginal itching or vulvar erythema.
- Avoid douching that is not needed douching interferes with the natural ecosystem and can cause excessive growth of lactobacilli that produce hydrogen peroxide.
- Keep a symptom diary: In my experience, an unnecessary douching habit and tracking your cycle can keep the exacerbation of your symptoms at bay, this is where you record when the irritation or discharge becomes worse, particularly around the luteal phase of your menstrual cycle, this will assist your physician to come up with the accurate diagnosis.
- Gentle vaginal alkalization: Baking soda sitz baths at home are safe and effective in raising the vaginal pH level and relieving pain.
- Good intimate hygiene: Rinse with plain water and keep the vulva dry as much as possible to reduce the vulvar oedema and irritation.
- Treat underlying conditions: Women with diabetes need to collaborate with their physician to maintain normal blood sugar level as this will help lessen repetition.
- Minimize the use of unnecessary probiotics: Too much probiotic supplementation can occasionally increase the symptoms by providing lactobacillus overgrowth syndrome.
Vaginal Symptoms: When to Visit a Doctor
See a doctor in case the discomfort lasts longer than two weeks, or when there is unusual bleeding or pain aggravation. Professional assessment can be used to eliminate other causes and ensure the diagnosis. The latency in care can extend the process of misdiagnosis of candidiasis and unnecessary treatment.
Conclusion
The best thing is that cytolytic vaginosis can be controlled. In my opinion, the timely diagnosis is the key to preventing months of pain and misdiagnosis. After the treatment, the symptoms tend to improve in two to three weeks and may not recur at all provided there are preventive measures taken. When women are taught how to follow their menstrual cycles and avoid things that they can predict, they usually prevent recurrence, which makes them enjoy a healthy vagina and a calm mind.
FAQs
1. Bacterial vaginosis and cytolytic vaginosis: What is the difference?
Bacterial vaginosis results in fishy smell and increased vaginal pH, whereas cytolytic vaginosis results in no smell and extremely low vaginal pH.
2. Will cytolytic vaginosis resolve itself?
In certain instances, the symptoms can go away with the period of menstruation, when in most cases the women require treatment to restore normal pH level.
3. What is the Wet smear method of diagnosis of cytolytic vaginosis?
Naked nuclei, cytoplasmic debris, and low vaginal PH are examined by doctors using a microscope and excluding yeast infections.
4. Is baking soda douche safe in the treatment of cytolytic vaginosis?
Yes, with the help of a doctor, baking soda douche can be used to increase vaginal pH and reduce symptoms in a few days.
5. Why do lactobacilli grow excessively in cytolytic vaginosis?
The lactobacillus overgrowth syndrome may be provoked by hormonal changes during the luteal phase, pregnancy, or excessive intake of probiotics.

 Medically reviewed by
Medically reviewed by