Learning about the difference between osteoporosis and osteoarthritis is the key to healthy aging. Although they have a similar effect on aging adults, they are not interchangeable. Osteoporosis is a condition of the bones, which causes the bone density to be lost, whereas osteoarthritis is a disease of the joints which is a result of cartilage destruction. When neglected, these conditions may cause pain, fractures and limited movement. This guide will tell you their causes and symptoms, risk factors, and their diagnosis and treatment choices so you can get steps toward stronger bones, better movement and more active and independent future.
Osteoporosis vs Osteoarthritis: Major Differences
Arthritis vs osteoporosis is confused as many believe that they are more common in elderly people. But one of the problems lurks within the bones and the other hits the joints. Osteoporosis causes loss of bone density, thus leaving the bones frail and easily fractured by even minor accidents. Osteoarthritis on the other hand is characterized by the breakdown of cartilage and degeneration of the joints resulting in stiffness, swelling, and pain.
| Condition | Primary Problem | Key Test | Main Effect |
| Osteoporosis | Weak, porous bones (bone resorption) | DXA scan | Increased fracture risk |
| Osteoarthritis | Worn-out cartilage in joints | X-ray imaging | Joint stiffness and reduced motion |
Practically 54 million humans in the U.S. have low bone density or osteoporosis and osteoarthritis occurs in approximately 32.5 million elderly individuals. This implies that millions are experiencing joint pains rather than bone losses and in some cases both.
Osteoporosis and Osteoarthritis Causes
Two of the most frequently encountered diseases in aging adults and older adults include osteoporosis and osteoarthritis, which have very diverse causes. Knowing the causes of these conditions would enable you to make healthier decisions and reduce the rate at which they occur. Osteoporosis gradual reduces the bones to the extent they break, whereas osteoarthritis erodes the cartilage in the joints causing pain and stiffness. They have certain overlapping triggers, but they possess their own risk factors, which are unique to them, and which involve different parts of the body.
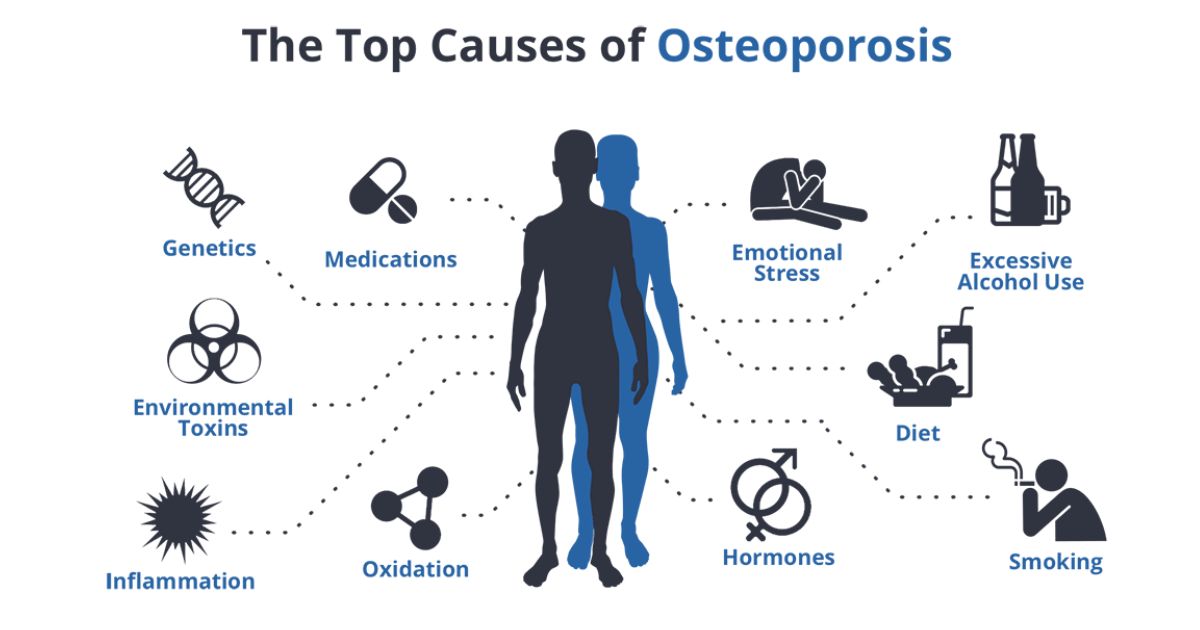
Hormonal Changes
Hormonal changes are usually the first signs of osteoporosis particularly in postmenopausal women. Estrogen is critical in controlling the remodeling of the bones, and once it becomes low, the bone deteriorates more quickly than it is being replaced. Men also may undergo slow loss of testosterone, which is associated with bone loss with age.
Deficiency of low Calcium / Vitamin D
The bones of your body are the bank, which keeps the calcium in them to help them be firm. When the food you are consuming does not contain sufficient calcium or vitamin D, your organism takes calcium out of the bones, leaving them less strong. In the absence of Vitamin D, calcium is not absorbed effectively resulting in osteopenia and ultimately osteoporosis.
Smoking Risk and Alcohol Use
Smoking and heavy drinking both disrupt bone-building cells and limit the absorption of calcium. Nicotine is a substance that slows down bone healing following fractures whereas alcohol is a substance that predisposes people to falls. These are the habits that are predominant causes of bone disease and should be dealt with at an early age to age well.
Long-Term Steroid Use
Steroid drugs such as prednisone, commonly prescribed to treat autoimmune disorders, do damage to the bones when used over months or years. They enhance bone resorption, and reduce calcium uptake, which results in an augmented risk of fracture. Another scenario in which the bone health of patients on long-term corticosteroids can be closely monitored is by the doctors.
Chronic Illnesses
Some chronic diseases – thyroid problems, celiac disease and kidney problems – upset hormone and mineral balances required to build strong bones. Bone disease and joint damage are also caused by diabetes and inflammatory diseases, which increase the general risk.
Wear and Tear on Joints
Osteoarthritis normally occurs because of the years of wear and tear of joints. The smooth cartilage that cushions bones becomes thinner with time resulting in friction. The result is stiffness, swelling, and pain in the joints which increases with activity but reduces with rest.
Prior Injuries
The degeneration of the joint may be accelerated by old sports injuries, fractures around a joint or even by surgery. Lacerated cartilage does not heal completely leaving the joint more exposed to premature osteoarthritis, particularly the knees and hips.
Obesity
Weight gain imposes undue pressure on weight bearing joints such as knees, hips and lower back. This mechanical overloading accelerates breakdown of cartilages resulting in earlier and more severe joint pain as opposed to bone loss issues.
Family History
Density of bone and structure of joints can be predetermined by genetics. There is a likelihood that you will have an increased risk of the same conditions as your parents or siblings had bone fractures or severe osteoarthritis, and thus fall prevention and early screening are even more crucial.
Lack of Exercise and Malnourishment
Osteoporosis and osteoarthritis become worse in case you live a sedentary life. The absence of weight-bearing exercise causes the weakening of bones and muscles and inadequate nutrition does not provide the building blocks of strong bones and good cartilage. Vital prevention is exercising and eating well.
Symptoms of Osteoporosis
Osteoporosis is referred to as the silent thief in that it takes away bone strength silently with time. The majority of aging adults do not experience pain until a bone fracture, hence the need to detect them early. It is possible to recognize the slightest variations in your body to take action when your movement is not restricted by the severity of the injuries.
- Minor fractures of the bones frequently due to minor falls.
- Gradual height loss
- Stooped posture
- Chronic back pain
- Weak grip strength
- Brittle nails (seen on DXA scan)
Symptoms of Osteoarthritis
However, osteoarthritis causes early manifestation as compared to osteoporosis. It normally starts with stiffness in the joints upon waking up or sitting down. The pain increases with movement, which usually involves knees, hips, hands, and spine, resulting in more and more of a decreased quality of life and independence.
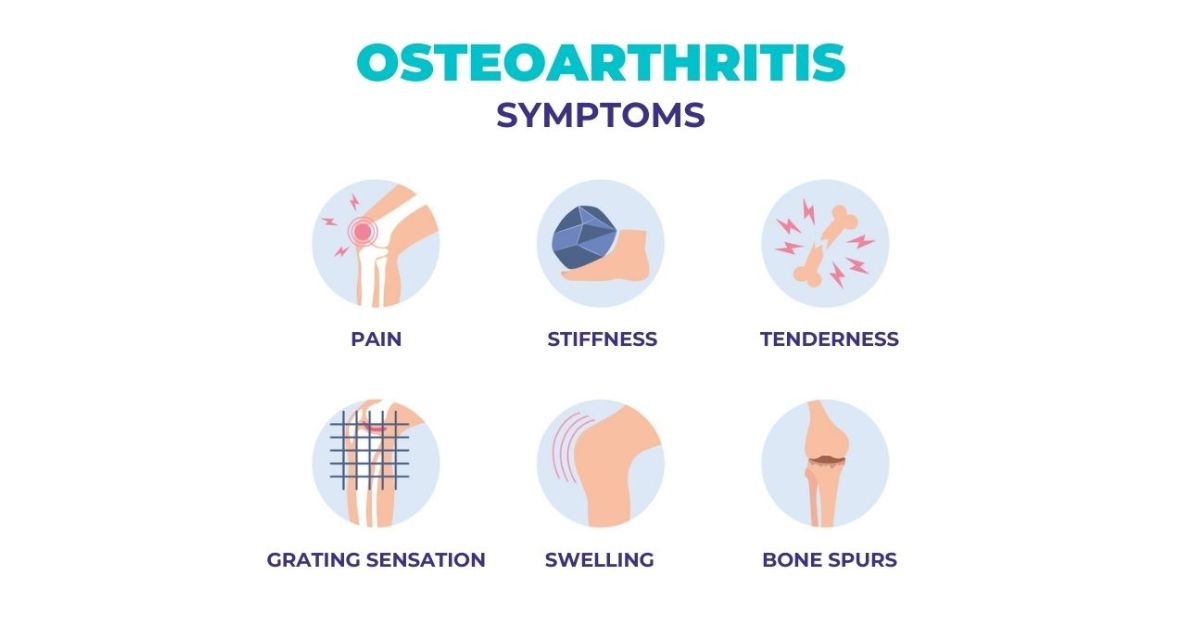
- Morning joint stiffness
- Pain during movement
- Swelling around joints
- Grinding or popping sounds
- Reduced joint function
- Gradual loss of mobility
- Difficulty climbing stairs
- Mobility impairment in the severe cases.
The influence of these conditions on Bones and Joints
Imagine osteoporosis as a house having crumbling walls the structure becomes weak and collapses internally. This weakening of the bones causes them to become brittle resulting in the breakage of these bones. Not only does this augment the risk of fractures but it also elevates the risk of occurrence of complications such as pneumonia or blood clots following hip fractures.
Osteoarthritis, on the other hand, is as though a door hinge that is wearing out. The cartilage degeneration eliminates the lubricated surface that smoothes movement. This leads to pain in movement and impaired joint performance becoming daily issues, slowly restricting mobility.
Risk Factors You Should Know
A number of risk factors are similar between both osteoporosis and osteoarthritis, and some are within your control, whereas others are not. Knowing the distinction can make you more emphasive on practices that secure your bones and joints as you age and are at increased risk of fracture.
Non-Modifiable Risks
- Age over 50
- Women gender (particularly the postmenopausal women)
- Bone or joint disease in the family history.
- Effect of genetics on bone resorption and joint structure.
Modifiable Risks
- Smoking risk
- Too much alcohol intake.
- Deficiency of low calcium / vitamin D.
- Sedentary lifestyle
- Weight gain and overweight.
Diagnosis: The Art of Telling Them Apart
The correct diagnosis is important as osteoporosis and osteoarthritis use very different methods of treatment. Prior to initiating a course of action, doctors use sophisticated imaging, medical history, and laboratory tests to identify a particular source of pain, stiffness, or fractures.
Osteoporosis Diagnosis
- DXA scan to determine bone mineral density.
- Evaluation of vertebral fractures of the hidden spinal fractures.
- Blood analysis (calcium, vitamin D, and hormones) analysis.
Osteoarthritis Diagnosis
- X-ray to identify bone spurs and narrowing of the joint spaces.
- MRI to closely view the cartilage and soft tissue.
- Physical examination in swelling, stiffness, and decreased joint functioning.
- Review of medical history of the past injuries or family history.
Therapy of Osteoporosis
The goal of treatment of osteoporosis is to improve bone strength, prevent bone fractures, and enhance the quality of life. With medication, supplement and lifestyle changes, bone resorption may be slowed down and the bone density rebuilt over time.
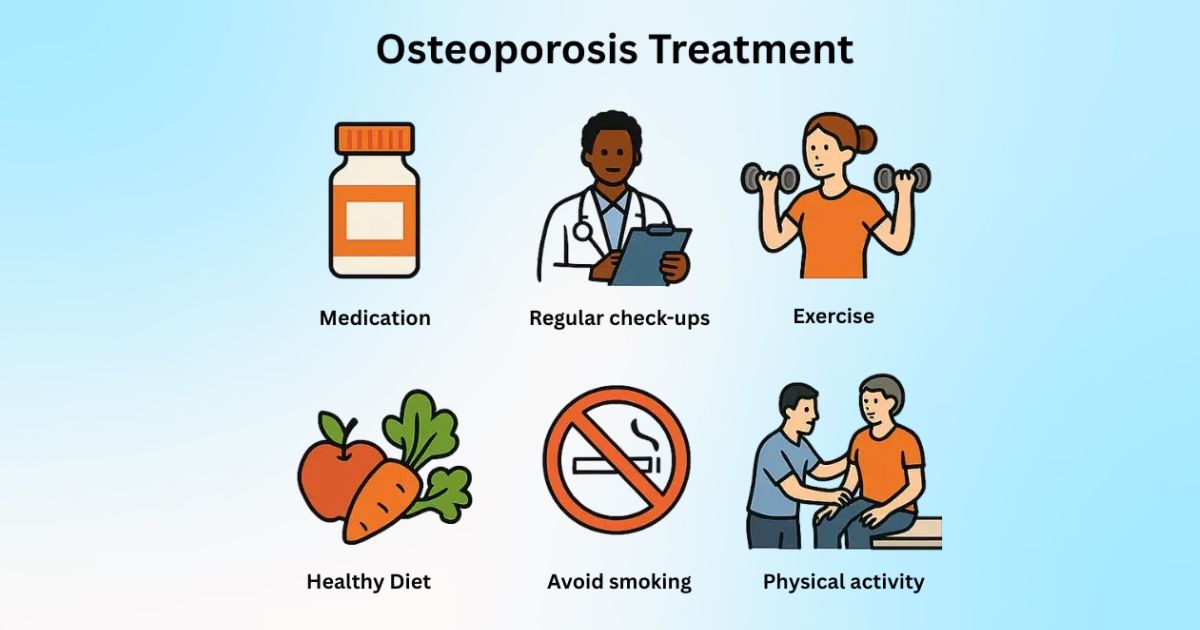
Medical Treatments
- Bisphosphonates to retard bone loss.
- Medications that lead to bone-building (teriparatide, abaloparatide, romosozumab).
- Vitamins (calcium, vitamin D) to improve bone mass density.
- Endocrine treatment of some postmenopausal women.
Lifestyle & Procedures
- Bone and strength training and weight-bearing exercise.
- Balance training in order to minimise fall risk.
- Healthy diet high in proteins, greens and dairy.
- Vertebroplasty or Kyphoplasty of painful vertebral fractures.
Osteoarthritis Treatment
The objective of treating osteoarthritis is to relieve the pain, reduce the degeneration of the joint, and keep you active. An integrated non-surgical and surgical program can be used to treat older adults with chronic joint pain to control symptoms and enhance their quality of life.
Non-Surgical Treatments
- Joint-friendly movement to be taught through physical therapy.
- NSAIDs or corticosteroid injections of pain.
- Loss of weight in order to decrease stress on knees and hips.
- Aids to mobility (canes, braces)
Surgical & Advanced Options
- Severe cases- joint replacement surgery.
- Newer hip and knee implants that are long-term.
- Rehabilitation after the surgery to get strength and range of movement.
Bone and Joint health Lifestyle Changes
Habits have a huge impact on day-to-day lives. Healthy bones are supported by a high dairy, leaf, and fortified food diet. Add this along with some exercise to strengthen your bones and joints walking, dancing, or yoga to make your body strong n in my opinion, yoga plus strength training will be the most effective.
At home, pay attention to fall prevention with grab bars, clear floors and enhanced lighting. In case of joints, opt to an exercise that is friendly to the joints such as swimming or cycling to maintain fitness without undue strain.
Averting Osteoporosis and Osteoarthritis
Early prevention is always best but it is never late either. Peak bone mass gained in the younger age and maintained through supplements (calcium, vitamin D) in the older age minimizes the risk of fractures. Preserve your joints through maintaining good exercise, preventing injuries, and maintaining a proper weight. I think that screening after the age of 50 is one of the smartest health investments you need to make.
Evidence-based programs are operating within communities across the U.S. to educate self-management education, balance training, and safe exercise routines to promote healthy aging. These programs are a good move towards a long-term wellness.
When to See a Doctor
Do not wait until a severe injury makes you take some action. When you experience unrelenting pain, pain in the hip, difficulty walking, see a doctor sooner. As in my case, early intervention after the initial symptom of back pain may help to avoid grave complications in future. The fractures are indicated by sudden back pain or height loss which requires immediate attention.
Urgent care is required immediately after a fall when the person is unable to stand due to the fact that untreated fractures may cause disability among the elderly. Early care enhances healing, maintains your mobility and protects your independence.
FAQs
1. How is osteoporosis and osteoarthritis different?
Osteoporosis leads to weak bones because of bone loss in terms of bone mineral density, and osteoarthritis impacts the joints leading to pain, stiffness, and degeneration of the joints.
2. Would you say that you can have both osteoporosis and osteoarthritis?
Yes old people have both conditions- a dual diagnosis- that makes them more prone to fractures and less able to move around.
3. What are the major risk factors of osteoporosis?
Risks are most important among postmenopausal women, family history, low levels of calcium / vitamin D deficit, lack of activities, risk of smoking and some medications.
4. Which is the most effective treatment of osteoarthritis pain?
The interventions include physical therapy and weight loss, pain management drugs, injections, and joint replacement surgery (severe cases).
5. What can I do to avoid osteoporosis?
To maintain healthy and strong bones, it is important to focus on weight-bearing exercise, bone strength training, a healthy nutrient-dense diet, and fall prevention measures.

 Medically reviewed by
Medically reviewed by