Do ADHD medications exacerbate the condition of dermatillomania? I believe this question is important, as it influences the life of so many people with skin picking disorder tend to pose when they have trouble with impulsivity and ADHD. Excoriation disorder is a type of the obsessive-compulsive spectrum whose dermatillomania impacts on everyday life. Because millions of people in the U.S. are dependent on drugs used to treat ADHD as well as stimulants, it is important to understand whether these medications enhance or aggravate picking behaviors. In this article, we will discuss research articles, case studies, treatment results, and management approaches to achieving a balance of care of ADHD and skin health.
What is Dermatillomania (Skin Picking Disorder)?
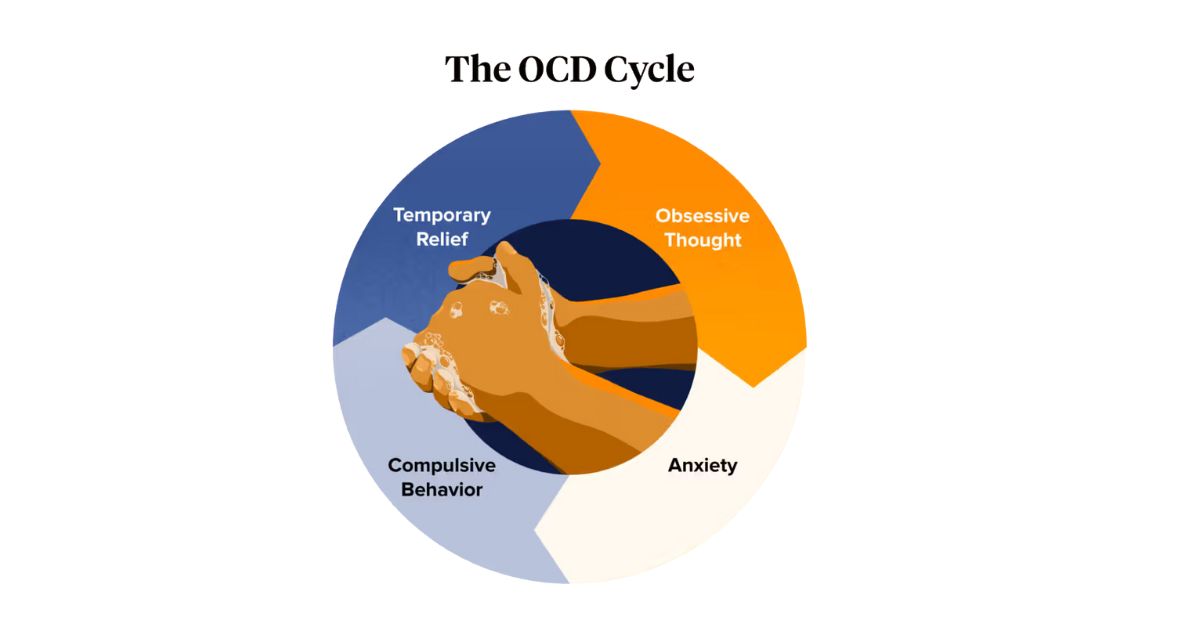
Excoriation disorder or dermatillomania is a mental disorder which is categorized as an obsessive-compulsive spectrum disorder. Individuals affected by this disorder scratch their skin repeatedly, which can result in wounds, scarring or infection. It is not just a habit but a tension/relief cycle that is similar to other impulsive control disorders.
Dermatillomania is not only a bad habit, but it has been associated with executive functioning and cognitive alteration in medical research studies. One case report, which was featured in psychiatric literature, showed that the outcome of the treatment frequently relies on the severity of psychiatric comorbidity like ADHD, anxiety, or OCD. According to many patients, the moment of temporary calmness after picking supports the cycle even despite the negative effects.
What is the relation between Dermatillomania and ADHD?
Comorbidity is the occurrence of ADHD and dermatillomania. All these are common characteristics that can be impulsive, hyperactive and inattentive, and thus prone to compulsive behaviors. To illustrate this, an individual with restless energy can be subconsciously inclined to repeat skin picking to relieve the stress.
Studies indicate that comorbid skin picking disorder with ADHD has an increased severity of symptoms than comorbid dermatillomania disorder alone. Actually, certain studies that employed impulsivity questionnaires, inattention and hyperactivity scales, and depression questionnaires show that people with ADHD score higher on the measures of compulsive behaviors. The results highlight the role of poor executive functioning in worsening self-harm behavior such as skin picking.
Do ADHD Drugs Cause or aggravate Skin Picking?
How dermatillomania might be affected by ADHD drugs is a question with no single-answer solution. Some patients state that they feel better by taking medication, and some have more urges. The trick is the stimulant drug like methylphenidate or amphetamines influences the dopamine and norepinephrine system of the brain.
Stimulants assist some persons in controlling their impulsive behavior, which results in less skin picking. Instead, to other people, these drugs increase arousal, make them more aware of skin flaws and stimulate picking. Follow-up appraisals and monitoring the response to treatment are clinical observations that indicate that the adverse effects may differ greatly in different patients.
Comparison of the effect of ADHD medication on Dermatillomania
| Type of medication | Potential effect on Dermatillomania | Notes |
| Stimulants (Ritalin, Adderall) | Potentially can increase picking in ADHD patients | Improves ADHD symptoms but can increase anxiety |
| Non-Stimulants (Atomoxetine, Guanfacine) | Less apt to aggravate picking | Useful in the comorbid |
| Behavioral Therapy (CBT, Habit Reversal) | Reduces picking urges directly | BEST with medication |
Stimulant Drugs (Ritalin, Adderall) and Dermatillomania
Ritalin (methylphenidate) and Adderall (amphetamine salts) are the most commonly used ADHD drugs which are stimulants. Such medications raise concentration since they boost dopamine, a neurotransmitter that is associated with motivation and reward-seeking. To most people, this results in improved academic performance, executive functioning and professional accomplishments. Nevertheless, since dopamine is involved in compulsive behavior, sometimes stimulants only aggravate the symptoms of dermatillomania.

A case report involved a patient who had ADHD and dermatillomania who was being treated using methylphenidate. Clinical observations revealed a decrease in symptoms of ADHD- especially inattention and hyperactivity scales but skin picking became worse. This example shows how a fine line can be between a better outcome of treatment of ADHD and a possible adverse outcome in excoriation disorder.
Ritalin (Methylphenidate)
Ritalin, or Methylphenidate, is commonly used as the initial management of ADHD. It inhibits the uptake of the dopamine and norepinephrine and raises their concentration in the brain. Although this makes one more focused and less impulsive, it can also make compulsive self-harm, such as skin picking, worse.
The responses of patients with psychiatric comorbidity are usually mixed. On the one hand, they claim the improvement of the symptom in school and work performance. On the other, they can see greater desires to pick, particularly at times of stress or anxiety. The behavior is mild and manageable in a few cases whereas it is clinically significant and needs to be adjusted to treatment in some cases.
Adderall (Amphetamine Salts)
Adderall, the mixed amphetamine salts, is both a dopamine and a norepinephrine stimulant. It has a longer-term stimulating effect than methylphenidate and is useful in the treatment of inattention and hyperactivity throughout the day.
Nevertheless, it has such a powerful impact on the reward system that at times, it aggravates the skin picking disorder. Patients can also become sensitive to small skin defects, resulting in the repetitive picking. It has also been reported that Adderall has a tendency of enhancing anxiety levels, which in turn indirectly contributes to compulsiveness. Close clinical observation and follow up assessment are important in order to differentiate between the normal side effects and the dangerous behavioral changes.
So Why do Stimulants Sometimes Intensify Skin Picking Behaviors?
Stimulants have the potential of enhancing pre-existing weaknesses. These drugs have an unwanted side effect of making the brain more sensitive to compulsive urges by boosting the level of dopamine. An individual can become hyper-attentive to minute details resulting in picking. Other individuals can develop anxiety brought about by stimulants, which drives them into self-damaging activities.
This can be imagined as the turn up of a radio. The volume assists you to hear crucial information but may likewise overwhelm with noise in the background. Simulators likewise enhance concentration but have the power to increase obsessive actions. This phenomenon has been argued to explain the worsening in symptom severity in response to general treatment receptivity in ADHD.
Non-Stimulant ADHD Drugs and Skin picking Disorder
Non-stimulant ADHD drugs are promising to patients with this problem of stimulant side effects. Such drugs as atomoxetine, guanfacine, and clonidine have different processes of controlling attention and impulsive control. It has been shown that they might not aggravate dermatillomania and sometimes they actually decrease self-harm behaviors.
Non-stimulants are often prescribed by clinicians when the stimulants present a psychiatric comorbidity complications. To illustrate the point, a patient whose increased picking is due to the use of stimulants might experience a reduction in symptoms upon changing drugs. The continued clinical scores and follow-ups are critical in leading these treatment adjustments.
Co-Occurring Conditions: ADHD, OCD and Dermatillomania
There are a lot of clinical intersections among the patients. ADHD, obsessive-compulsive disorder, and dermatillomania tend to coincide, and they make a complicated diagnostic picture. Research indicates that between 25 and 30 percent of all people with ADHD have symptoms of obsessive-compulsive spectrum.
This overlap makes the treatment difficult. A psychiatrically comorbid patient might react to drugs in a different manner. As an example, medications used to treat ADHD can exacerbate the picking of OCD. It is due to this that the treatment plans and close clinical observation are imperative in the management of comorbid psychiatric disorders.
Symptoms that Have Given the Impression ADHD Meds Only Makes Skin Picking Worse
In any case where ADHD drug leads to dermatillomania, there are some warning signals that are evident. Patients can report more time spent picking, higher wound severity or infection. After an increase or decrease in dose, families tend to see an increase in levels of distress or more observable scars.
Anxiety questionnaires, impulsivity questionnaires, and clinical monitoring tools are frequently used by doctors to monitor these symptoms. When the treatment outcome indicates the augmentation of dermatillomania regardless of the enhancement in the cognition of ADHD, then a reassessment is crucial. Patients are never supposed to discontinue medication without consulting with their provider.
Moderation Strategies of the ADHD Patients with Skin Picking Disorder
ADHD and dermatillomania are both conditions that need a complex treatment. Besides drug, behavioral therapy forms a part of the treatment. Such methods as habit reversal training, cognitive-behavioral therapy, and acceptance-based techniques can assist the patient to break the picking cycle. Having tried both used together, I find habit reversal therapy to be more effective in combination with mindfulness.
A study mentioned by the American psychological association found that CBT resulted in the improvement of symptoms in 52-60 percent of patients with excoriation disorder. Urges can also be decreased by simple techniques such as the use of fidget objects, applying bandages, or doing mindfulness. Medication adjustments plus therapy is the most effective way of treatment.
Other ADHD Treatment in Case of Worsening Skin Picking
In cases where skin picking is worsened by stimulants, there are other options of ADHD therapy. As mentioned above, a non-stimulant can be used. Also, aspects like lifestyle changes like exercise, sleep improvements, and dietary changes contribute to reducing the regularity of attention and compulsive behaviors.
Other clinicians consider nutritional supplements, such as omega-3 fatty acids, which show small effects on ADHD cognition and executive functioning. Finally, treatment must be very personalized, and close follow-up assessment and reporting of all side effects during medical appointments.
When to Discuss ADHD Medications and Dermatillomania to a Doctor
Patients need to visit a doctor in case the skin picking becomes worse when the ADHD medication is started or changed. Symptoms include blood loss, obvious scars, recurring infections or mood swings. There are dose adjustments, change of medication, and inclusion of behavioral therapy that may be suggested by clinical professionals.

Medications, as one psychiatrist described it are a means and not a panacea. It is time to reconsider the plan in the instance where side effects overshadow the advantages. Such discussions make sure that ADHD and dermatillomania are treated in an effective manner without putting one over the other.
Conclusions
Then, will the dermatillomania be aggravated by ADHD medications? The answer is complicated. To others, stimulants enhance impulse control and decrease picking. To others, they increase the severity of symptoms and cause unfortunate effects. The middle ground is in close clinical follow-up, integration of behavioral therapy, and free communication between the patient and the provider. This is all a matter of equilibrium, in my opinion, medications are needed, but therapy puts the puzzle together.
ADHD and dermatillomania are both treatable. Patients can enjoy healthy lives with the combination of appropriate reaction to the treatment, therapy, and personal choices of the medication. The process is not always easy, but with individual treatment, it is possible to recover.
FAQs
Do medications used to treat ADHD such as Ritalin or Adderall aggravate the skin picking disorder?
Yes, there are occasional cases in which stimulant medications can increase urges, but there are also cases where patients can improve their symptoms.
What can be the reason that ADHD comorbidity poses a higher risk of dermatillomania?
ADHD patients are more likely to engage in compulsive skin picking because of their shared characteristics such as impulsivity, inattention, and executive function problems.
Do non stimulant ADHD drugs prove safer in excoriation disorder?
A non-stimulant drug like atomoxetine or guantanamine is less prone to aggravating picking behaviors and can be beneficial to certain patients.
What is the role of the therapy to treat ADHD and skin picking disorder?
CBT and habit reversal training are behavioral therapies that make people control their impulses and minimize compulsive picking.
At what point can somebody approach the doctor regarding ADHD medications and skin picking?
When medication aggravates self-harm, becomes infected, or increases anxiety, then it is time to talk to a healthcare professional about other options.

 Medically reviewed by
Medically reviewed by