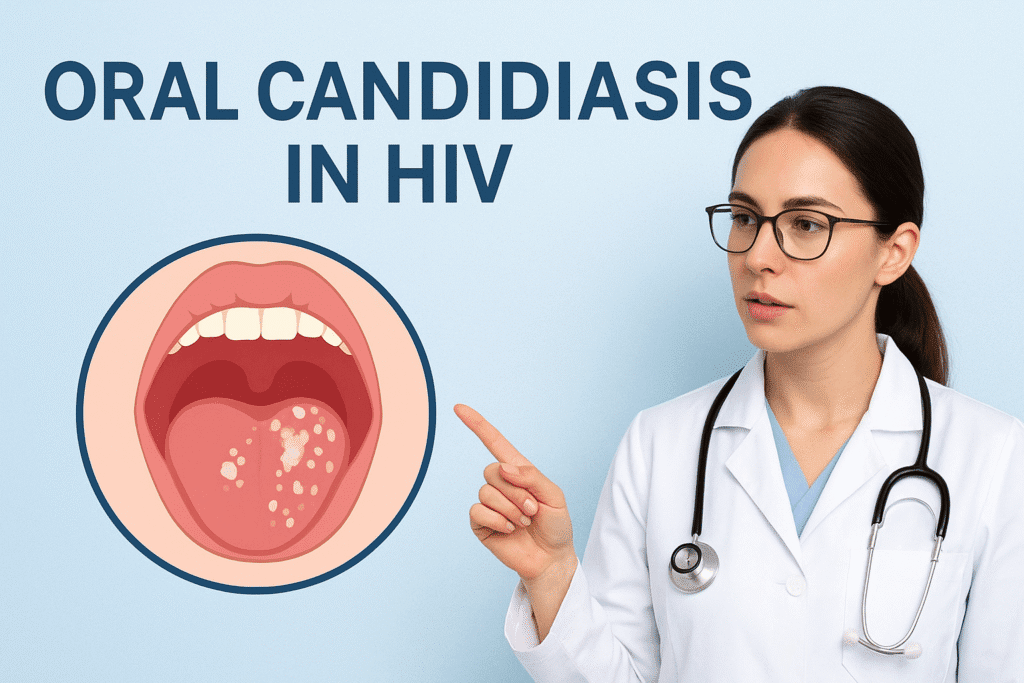
HIV is not only accompanied by challenges other than the virus itself, and oral candidiasis, also known as oral thrush, is one of the most prevalent opportunistic infections among people with HIV/AIDS. It is a disease that develops when a fungus known as Candida proliferates in the mouth, leading to the development of white or red spots, pain, and difficulty eating.
Although oral candidiasis might appear to be an insignificant infection at the outset, it has significant consequences for general health, nutrition, and quality of life among HIV-positive individuals. It is essential to understand the causes, symptoms, and methods for controlling and preventing it to maintain good health and avoid complications.
What is Oral Candidiasis?
Candida is a type of fungi infection that is often caused by Candida albicans. It is an organism that is usually present in small quantities in the mouth, digestive tract, and skin of healthy persons without any complications. Nevertheless, Candida may develop in excess amounts in case the defence system is weakened or when the natural balance of microorganisms is disrupted. Oral candidiasis is not only an oral health problem in people with HIV, but it is also frequently a clinical indicator of immunosuppression. Sometimes its appearance may indicate the development of HIV disease and the necessity of immediate medical treatment.
Why is Oral Candidiasis Common in HIV?
HIV attacks and kills T cells (CD4+) of the body, which plays a crucial role in combating infections. A decrease in the CD4 count compromises the immune system to deal with fungal organisms such as Candida. This provides a habitat where the fungus can thrive resulting in infection. The presence of several risk factors predisposes people with HIV to oral candidiasis, such as large viral load, low oral hygiene, use of many medication types that cause a dry mouth, use of antibiotics frequently, nutritional deficiencies, and smoking or alcohol consumption. This is why oral candidiasis can be regarded as one of the most common opportunistic infections in HIV and may be developed at the initial stages of immune deficiency.
Types of Oral Candidiasis in HIV
Oral candidiasis may have various clinical manifestations with their different features. The most prevalent are:
Pseudomembranous Candidiasis
Pseudomembranous Candidiasis commonly known as thrush, which is characterised by creamy white spots on the tongue, the inner cheeks or the gums. These patches are wiped off, and there may be areas of redness or bleeding.
Erythematous Candidiasis
Erythematous Candidiasis is characterized by painful reddening of the interior of the mouth and is linked to a burning sensation, particularly when consuming hot or sour foods.
Hyperplastic Candidiasis
In Hyperplastic Candidiasis where thick white plaques, which are hard to get rid of, can appear and resemble precancerous lesions. Localised version, known as angular cheilitis, is cracks, soreness, and reddening of the corners of the mouth that can be extremely uncomfortable.
Symptoms of Oral Candidiasis in HIV
Mild Symptoms
- White or reddish patches inside the mouth (tongue, inner cheeks, gums, or palate).
- Soreness or burning sensation in the mouth.
- Unpleasant or altered taste (loss of taste, metallic taste).
Moderate Symptoms
- Pain or discomfort while eating or drinking.
- Cracks or fissures at the corners of the mouth (angular cheilitis).
Severe Symptoms
- Difficulty swallowing (dysphagia).
- Chest pain or the sensation of food getting stuck.
- Esophageal candidiasis (infection spreading to the throat or esophagus, indicating severe immunosuppression).
How to Diagnose it?
Clinical Examination
- In most cases, diagnosis is made through a simple clinical examination.
- The characteristic white or reddish lesions inside the mouth are usually sufficient for identification.
Microscopic Examination or Culture (if needed)
- In unclear or ambiguous cases, a small sample (oral swab or scraping) may be collected.
- The sample can be examined under a microscope or cultured in the laboratory to confirm the presence of Candida species.
Endoscopic Evaluation (for suspected esophageal candidiasis)
- If the infection is suspected to have spread to the esophagus, an endoscopic test may be required.
- This helps assess symptoms like difficulty swallowing or chest discomfort.
Evaluation of Immune Status
- Recurrent or persistent oral candidiasis is an important clinical indicator in HIV patients.
- Doctors often recommend checking CD4 cell counts and viral load to assess the immune system status.
Common Treatments
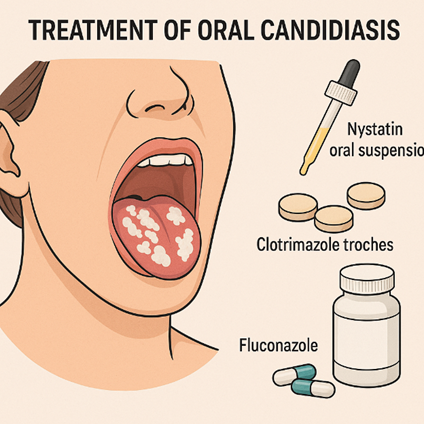
The severity and recurrence of infection determine the treatment. In cases of mild infections, topical antifungal agents like nystatin mouth rinses or clotrimazole lozenges are typically given out and these solutions tend to heal the infection in just a few weeks. But in moderate to severe, or if the occurrence of thrush is frequent, systemic antifungal agents like fluconazole are employed since they are systemic and able to penetrate more deeply affected foci.
Other options such as itraconazole or voriconazole, can be required in cases that are more resistant. In case of esophagus extension, there should be a systemic antifungal therapy. This is because when antifungal is used frequently, it may cause drug resistance, and therefore it is significant that medication use is closely supervised by a health care provider.
| Condition | Treatment Approach | Examples | Notes |
|---|---|---|---|
| Mild infections | Topical antifungal agents | Nystatin mouth rinses, Clotrimazole lozenges | Usually heal within a few weeks |
| Moderate to severe or recurrent infections | Systemic antifungal agents | Fluconazole | Penetrates deeper infection sites |
| Resistant cases | Alternative systemic antifungals | Itraconazole, Voriconazole | Used when infection does not respond to first-line therapy |
| Esophageal extension | Systemic antifungal therapy | Fluconazole or alternatives | Required due to deeper infection |
| Important consideration | Supervised medication use | — | Frequent antifungal use may cause drug resistance; close monitoring is essential |
Role of Anti-Retroviral Therapy (ART)
The treatment depends on the seriousness and frequency of infection. Topical antifungal agents such as nystatin mouth rinses or clotrimazole lozenges are usually administered in cases of mild infections and such solutions are likely to cure the infection within a few weeks. However, in moderate to severe, or where the incidence of thrush is recurrent, systemic anti-fungal agents such as fluconazole are used because of their systemic nature and their ability to serve more deeply involved foci.
It may require other alternatives like itraconazole or voriconazole in more resistant cases. Systemic antifungal treatment should be present in case of esophageal extension. This is because in situations where antifungal is administered regularly, there are chances of developing drug resistance and hence drug administration must be closely monitored by a health care provider.
Self-Care and Lifestyle Tips
Besides medical intervention, lifestyle interventions contribute significantly to the prevention and management of oral candidiasis. Proper oral hygiene is a necessity and consists of brushing teeth regularly, using floss, and mild mouth rinses. There are habits to avoid, like smoking and consuming large quantities of alcohol, that make fungal growth decrease. Immune functionality could be maintained with the help of a balanced diet, high in vitamins and minerals, whereas the consumption of sugary foods and refined carbohydrates suppresses the development of Candida.
It is also important to be well-hydrated and take good care of dentures, cleaning them every day and taking them out at night. By conducting regular checkups, dental issues may be identified in their initial stages and complications.
Coping and Support Mechanisms for Living with HIV Thrush
Oral candidiasis impacts not just physical well-being but also has psychological and social effects. The presence of visible white patches or cracked lips can lead to feelings of self-consciousness, while discomfort during eating may restrict food options and diminish the enjoyment of social meals. Over time, this can result in decreased self-esteem and increased feelings of isolation. Reaching out for support from healthcare professionals, nutritionists, and HIV support groups can offer both medical advice and emotional comfort. Learning about oral candidiasis enables individuals to identify symptoms early, act swiftly, and avoid further complications.
Prevention Strategies for Oral Candidiasis in HIV
1. Adhere strictly to antiretroviral therapy (ART) to boost the immune system.
2. Monitor CD4 counts and viral load regularly to detect early signs of immune decline.
3. Attend routine oral health screenings during HIV care visits to catch thrush in its early stages.
4. Maintain good nutrition to support overall health and immunity.
5. Practice proper oral hygiene (regular brushing, flossing, and dental check-ups).
6. Avoid risk factors like smoking which increase the likelihood of infection.
7. Seek early treatment even for mild symptoms to prevent progression to severe or complicated forms.
Conclusion
Oral candidiasis in individuals with HIV is not just a simple mouth infection—it serves as an indicator of weakened immunity and can often be the initial sign of advanced HIV disease.
Although it is one of the most prevalent opportunistic infections among those who are HIV-positive, it is both preventable and treatable. Antifungal treatments are effective in clearing up infections, but the best way to maintain long-term control is through the regular use of antiretroviral therapy, which helps to restore immune function.
By maintaining good oral hygiene, making healthy lifestyle choices, and sticking to ART, individuals living with HIV can significantly lower their chances of developing oral candidiasis, enhance their comfort, and improve their overall quality of life.
FAQ’s
1. Is oral candidiasis contagious?
Oral candidiasis is generally not contagious. Candida is a prevalent fungus found in the body, and infections typically arise when the immune system is compromised rather than through contact with others.
2. Does oral thrush mean HIV is advanced?
Oral thrush frequently signifies a weakened immune system, particularly when it is persistent or severe. However, the best way to evaluate disease progression is through CD4 count and viral load tests.
3. Can thrush go away on its own?
In some mild instances, thrush may resolve without treatment, but for individuals with HIV, it usually necessitates antifungal medication to avoid worsening or recurrence.
4. What foods help against thrush?
A diet that restricts sugar and refined carbs while incorporating vegetables, lean proteins, and probiotic-rich foods like yogurt can support a healthy oral environment.
5. Can oral candidiasis return after treatment?
Yes, recurrence is quite common if HIV is not effectively managed. Sticking to ART and adopting preventive lifestyle habits significantly lowers the chances of repeated episodes.

 Medically reviewed by
Medically reviewed by