Oral thrush is also called pseudomembranous candidiasis, which is one of the most well-known types of mucosal candidiasis of the mouth and throat. Most people are infected with Candida albicans, a normal fungal resident of the mouth that may proliferate and cause infection when the human defence system is weak. The disease manifests itself in the form of cottage cheese-like white spots in the mouth that can be wiped off with ease, leaving a reddish or red mucosal lining behind. Oral thrush is typically mild and non-progressive, but it may indicate underlying health conditions, including immunosuppression, uncontrolled diabetes mellitus or long-term use of antibiotics or steroids.
Understanding Pseudomembranous Candidiasis
Pseudomembranous candidiasis is a type of oral candidiasis that has a number of clinical forms, such as chronic hyperplastic candidiasis, erythematous candidiasis, and denture stomatitis. The most acute and recognisable of those is the pseudo membranous one. The condition is a result of Candida albicans which is the microbe normally found in small amounts in the oral microbiota but which grows in excess due to an altered balance between the immune defence of the host and the microbial flora. This imbalance usually occurs with the intake of broad-spectrum antibiotics or inhaled corticosteroids without maintaining good oral cleanliness and results in the overgrowth of fungi.
Causes and Risk Factors
Pseudomembranous candidiasis can be caused by several factors. The most common include:
- Extended course of antibiotic treatment that disturbs the balance of bacterial flora in the mouth.
- Use of inhaled steroid medications in the treatment of asthma or COPD without subsequent rinsing of the mouth.
- Poorly managed diabetes, as high sugar in the blood favours the growth of fungi.
- Continuous or insufficiently cleaned dentures, which causes denture stomatitis.
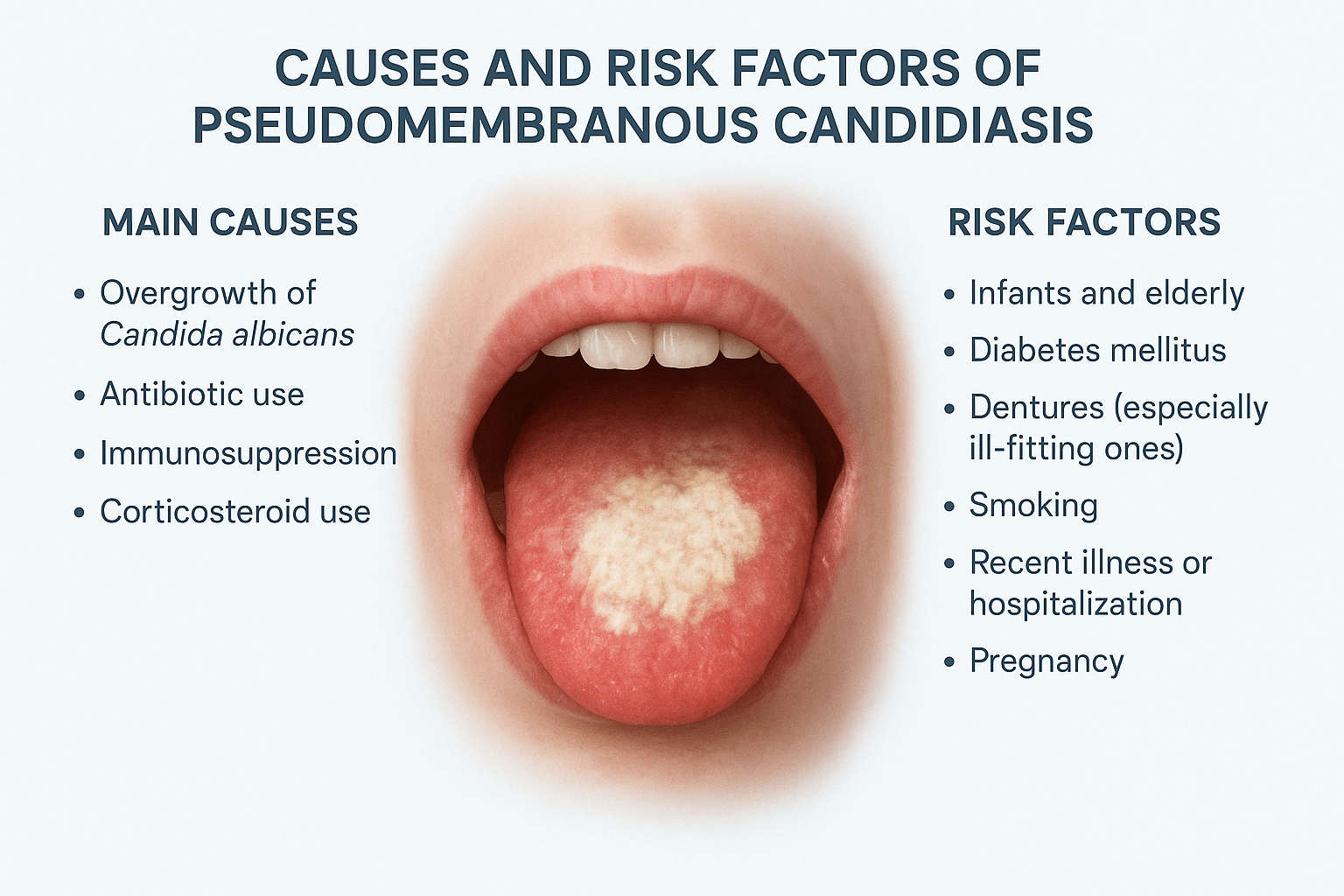
Other contributing factors and risks include:
- Nutritional deficiencies
- Xerostomia (dry mouth)
- Smoking
- Cancer treatment
- Use of immunosuppressive drugs
Neonatal thrush in neonates develops as a result of an inadequate immune response and can be transmitted between the infant and mother during breastfeeding.
Immunosuppressed individuals and those with thrush experience more severe and recurrent episodes; therefore, early diagnosis and treatment of the condition are important.
Clinical Features and Symptoms
Characteristic of pseudomembranous candidiasis is the development of creamy, curd-like white plaques in the mouth, usually on the tongue, inner cheeks, palate, and occasionally the throat or oesophagus. These lesions may be scraped off gently, exposing an erythematous or bleeding surface beneath.
The disorder can lead to:
- Pain
- Burning sensation
- Metallic taste
In certain cases, particularly where the infection extends to the oesophagus, swallowing can be difficult or food can feel like it is getting stuck in the throat, leading to Candida esophagitis.
Additional symptoms include:
- Taste changes (dysgeusia)
- Pain when eating acidic or spicy foods
In infants, thrush may cause:
- Irritability
- Refusal to feed
- Coincident diaper rash due to Candida
Atrophic candidiasis occurs in adults who wear dentures, as soreness develops under the denture base. It is essential to recognise these various presentations to diagnose and effectively manage the condition.
Diagnosis of Oral Thrush
Diagnosis is usually made clinically, by visual examination of the typical plaques. Nonetheless, recurrent or atypical cases may require laboratory confirmation. The presence of Candida albicans infection can be proven by a simple KOH smear of the lesion showing budding yeast cells and pseudo hyphae under the microscope. The Candida species can be detected on culture in Sabouraud agar or CHROMagar, and this is significant when antifungal resistance is suspected.
In patients with recurring or chronic infection, additional exploration of underlying systemic illness is justified. Blood glucose screening is used to exclude diabetes mellitus, and in high-risk individuals, HIV screening is advised. Patients who experience frequent Thrush attacks should have a medical check-up to determine potential defects in their immune system or underlying chronic illness that can predispose them to infection.
Treatment and Antifungal Therapy
Antifungal therapy with correction of predisposing factors is the mainstay of treatment of pseudomembranous candidiasis.
Topical Antifungal Therapy
In mild cases, topical antifungals are most often effective. The medications most frequently prescribed are:
- Nystatin oral suspension (swish and swallow)
- Clotrimazole troches, which need to be taken multiple times daily for 1–2 weeks
These agents act directly on fungal cells in the mouth, which reduces the number of systemic side effects.
Systemic Antifungal Therapy
Systemic antifungal agents, such as fluconazole or itraconazole, may be required in more serious or chronic cases, for example, those related to immunosuppression or Candida esophagitis.
In cases of resistant infections or non-albicans Candida strains, echinocandins or amphotericin B are used under expert medical care.
The Infectious Diseases Society of America (IDSA)
IDSA emphasises that the appropriate identification of fungal species is crucial to promote the optimal choice of antifungals and prevent resistance. Other recommendations to patients include keeping the mouth hygienic, dentures must be removed at night and the mouth after taking steroid inhalers to avoid reinfection.
Preventive Oral Care
It is sometimes possible to prevent pseudomembranous candidiasis by simple behavioural and oral hygiene measures. Individuals who take inhaled steroids are advised to wash their mouth with water or mouthwash after every intake of steroids to limit the local build-up of steroids to prevent fungal growth. Denture users are advised to wash dentures every day and leave them in antifungal or chlorhexidine solutions overnight. In order to minimise the chances of denture stomatitis, it is necessary not to wear dentures at night.

Glycemic control of diabetes, limiting unnecessary use of antibiotics and smoking cessation are also useful in reducing recurrence. In infants with neonatal thrush, the baby and the breastfeeding mother should be treated in tandem to avoid recurrence of the infection. Pacifiers and bottle nipples should be properly cleaned.
Special Considerations in Infants and Immunocompromised Patients
Oral candidiasis is most prone to infants, elderly people, and people with compromised immunity. Neonatal thrush will typically heal with topical antifungals, but repeat infections can be a sign of mother-to-child and/or equipment contamination.
Pseudomembranous candidiasis may be one of the first signs of immune deterioration in individuals with HIV/AIDS or in those receiving chemotherapy. The National Centre of Biotechnology Information (NCBI) found out.
One of the initial clinical symptoms of untreated HIV infection is oral candidiasis. These patients may need prolonged antifungal therapy and systemic therapy, and treatment of the underlying immunodeficiency by either antiretroviral or supportive therapies.
Complications and Prognosis
Though the majority of oral thrush cases are mild and self-limited, the infection can propagate further into the pharynx or oesophagus, causing Candida esophagitis. In cases of severe immunosuppression, Candida may be introduced into the bloodstream, resulting in systemic candidiasis, which can be fatal. Hence, early diagnosis and appropriate management are essential.
Prognosis and Follow-Up
The outcome is usually very good with proper antifungal treatment and management of existing risk conditions. However, reoccurrence is frequent when underlying factors such as:
- Poor inhaled steroid oral hygiene
- Uncontrolled diabetes
- Neglect of denture care
Regular follow-up visits to a dentist or physician are recommended to maintain oral health and prevent recurrence.
Conclusion
Oral thrush or pseudomembranous candidiasis is a frequent but under-recognised fungal infection of the mouth. It is a window into general health, indicating potential underlying conditions, including immunosuppression, diabetes, or a nutritional deficiency. Early antifungal therapy, proper oral hygiene and prevention measures make the infection easy to treat. Awareness of risk factors, awareness of symptoms, and adherence to the recommendations of trusted providers, such as the CDC, NHS, MedlinePlus, and IDSA, can enable patients and medical professionals to control the disease.
Good dental practices, medication control, and understanding of one’s own immunity health can reduce the occurrence of oral thrush, so all people can have healthy and comfortable mouths.
FAQ’s
What can lead to oral thrush?
Antibiotic use, disruption in the normal bacteria; inhaled steroid oral hygiene neglect; poorly controlled diabetes; denture stomatitis; and immunosuppression by HIV/AIDS, chemotherapy, or organ transplants are the most common causes of oral thrush. Anything that disrupts balance between the oral microflora and immune system may enable the growth of Candida albicans infection.
What are the typical manifestations of pseudomembranous candidiasis?
Symptoms are white or yellow spots on the tongue, inner cheeks or throat, painful sensation, loss of taste, and in some cases difficulty in swallowing. In the worst scenario, the infection can reach the esophagus resulting in candida esophagitis that causes chest pain or pains during swallowing.
Is oral thrush contagious?
Pseudomembranous candidiasis itself is not believed to be very contagious in normal adults. Nevertheless, Candida may be transmitted by direct contact, including kissing or breastfeeding, particularly when the immune system is compromised. Both the mother and baby may develop neonatal thrush which spreads through the nipple to the baby during feeding.
Will oral thrush resolve itself?
Mild cases of oral thrush spontaneously resolve, particularly in the cases of infants. Nevertheless, in adults, especially those who are diabetic, on steroids, or immunosuppressed, treatment is necessary to avert or reduce progression or recurrence. Neglecting symptoms may cause the infection to further get further into the throat or bloodstream.
And when do I see a doctor about oral thrush?
Consult medical attention when the symptoms last longer than 10-14 days, continue to recur, or when the symptoms are accompanied by pain during eating or swallowing. Those with weakened immunity are more likely to have invasive candidiasis and should not delay consultation because this may include people undergoing chemotherapy, those with HIV, etc.

 Medically reviewed by
Medically reviewed by