A stroke, often called a brain attack, happens when the blood flow to the brain is suddenly blocked or when a blood vessel on the surface of the brain bursts. From my experience working in healthcare, I have seen how quickly this medical emergency can change a person’s life. A stroke shares similarities with a heart attack, but instead of affecting the heart, it damages the brain tissue. It’s one of the fifth leading causes of death and adult disability in the United States, making it a major disease worldwide and the second leading cause of death globally.
When blood circulation is stopped or reduced, the brain doesn’t get enough oxygen or nutrients. As a result, brain cells begin to die within minutes, and without timely treatment, this can lead to permanent brain damage. Depending on whether the blood vessel is fully blocked, partly blocked, or has ruptures or leaks, the effects can differ. Some patients experience ischemic stroke, caused by blocked arteries or thrombotic occlusion, while others suffer hemorrhagic stroke, which involves bleeding, swelling, and inflammation inside the brain.

Prevalence of Brain Attack
In the U.S., over 800,000 people experience strokes each year, and about 82–92% of them are ischemic strokes. The annual cost of stroke care exceeds $72 billion, with direct medical costs projected to rise to $184.1 billion by 2030 due to the aging population between 65 and 79 years. Americans can prevent many of these cases by recognizing the signs, calling 911, and getting urgent medical help in a hospital setting.
Non-Hispanic Black adults and Pacific Islander adults face nearly twice the death rates as White adults due to disparities and risk variation.
Here’s a quick overview:
- The patients’ stroke accounted for 1 in 6 deaths (17.5%) related to cardiovascular disease.
- The death rate dropped slightly from 39.5 per 100,000 to 39.0 per 100,000 in 2023, but the risk remains significant.
- Every 40 seconds, someone experiences a stroke and every 3 minutes 14 seconds, another dies.
Each year, about 8000,000 people in the U.S. are affected:
- 610,000 are first strokes or new strokes.
- 185,000 are recurrent strokes (about 1 in 4).
Other Names People often Use for Stroke
- Brain attack
- Cerebrovascular accident (CVA)
- Cerebrovascular disease
- Cerebral infarction
- Cerebral apoplexy
- Acute ischemic stroke (AIS)
- Ischemic stroke
- Haemorrhagic stroke
- Stroke syndrome
Types of Stroke
During my clinical training, I realized how strokes can strike suddenly, affecting how the brain receives blood and oxygen. Understanding their types helps in early detection and timely care.
There are several main types of stroke, each with different causes and effects:
1. Ischemic Stroke (Clots)
Makes up 87% of all strokes. It occurs when a blood vessel is obstructed by clots, plaque, or fatty substances that narrow the arteries.
- Thrombotic stroke: A clot forms directly in a cerebral artery.
- Embolic stroke: A plaque fragment or embolus travels from the heart or large arteries to the brain.
- These blockages reduce oxygen and nutrient supply, causing brain tissue damage and cell death.
- Reperfusion therapy may help restore blood flow, rescuing viable tissue if done within the reperfusion window.
2. Hemorrhagic Stroke (Bleeds)
Caused by a weakened blood vessel that ruptures and bleeds into or around the brain.
- Common triggers: aneurysms, arteriovenous malformations (AVMs), and uncontrolled high blood pressure.
- Leads to intracranial pressure, swelling, edema, and tissue compression, damaging neurons and brain regions.
Subtypes include:
- Intracerebral hemorrhage – bleeding within brain tissue.
- Subarachnoid hemorrhage – bleeding in the subarachnoid space near the arachnoid layer.
3. Transient Ischemic Attack (TIA)
Often called a mini-stroke or warning stroke.
- Caused by a temporary clot or short-term interruption in blood flow.
- Symptoms may include weakness, vision loss, difficulty speaking, or imbalance that lasts 20 minutes to one hour.
4. Cryptogenic Stroke
A stroke where the cause can’t be determined even after tests like brain imaging (MRI).
5. Brain Stem Stroke
Affects the brain stem, often impacting both sides of the body.
- May cause paralysis, speech loss, or a locked-in state where the patient is unable to move or speak.
Symptoms and Warning Signs
When a stroke strikes, every second matters. It happens when the brain doesn’t get enough oxygen or fresh blood, leading to loss of muscle control, weakness, or even paralysis on one side of the body. In my experience working with stroke patients, I’ve seen how quickly the area of the brain it affects can change everything from speech to vision, to how someone moves or even thinks. That’s why recognition and early intervention are everything; the critical time to act begins the moment symptoms appear.
Some symptoms may seem small at first but can rapidly worsen. You might notice trouble speaking, slurred speech, or garbled words known medically as aphasia or dysarthria. Others may develop blurry vision, double vision (diplopia), or even vision loss in both eyes. Dizziness, vertigo, and loss of coordination (ataxia) often lead to stumbling or clumsiness. Many also experience sudden severe headaches, nausea, or vomiting with no known cause, and in severe cases, passing out, fainting, or even coma can follow. Subtle mood swings, confusion, amnesia, or personality changes can also occur especially when brain cells start to die due to disrupted blood flow.
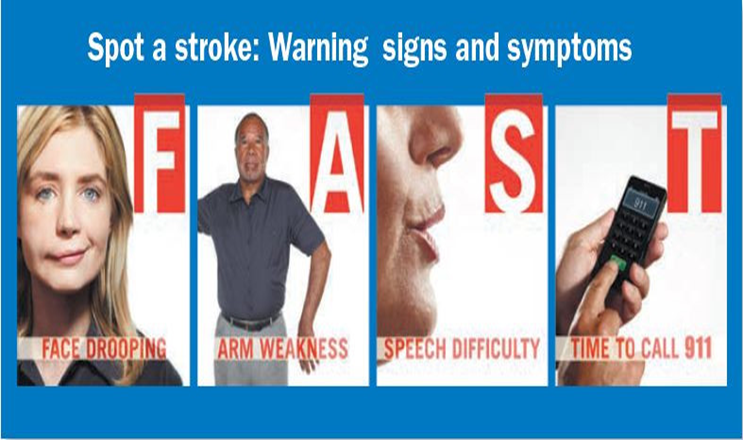
To quickly recognize a possible stroke, I always teach the BE FAST method a simple acronym that truly saves lives:
- B – Balance: Is there loss of balance or trouble walking?
- E – Eyes: Is there vision loss or blurred sight in one or both eyes?
- F – Face: Ask for a smile does one side droop?
- A – Arms: Can they raise both arms, or does one drift downward?
- S – Speech: Is their speech slurred, strange, or full of trouble choosing words?
- T – Time: Note the time when symptoms start and call for help immediately. Every moment without treatment reduces the chances of successful recovery.
Even if symptoms go away after a brief duration, such as with a transient ischemic attack (TIA) or mini-stroke, don’t ignore them. I’ve met people who felt “fine” after a few minutes but later faced a full stroke within a year. TIAs may clear up, but they’re a serious condition that demands medical help.
Stroke Risk Factors
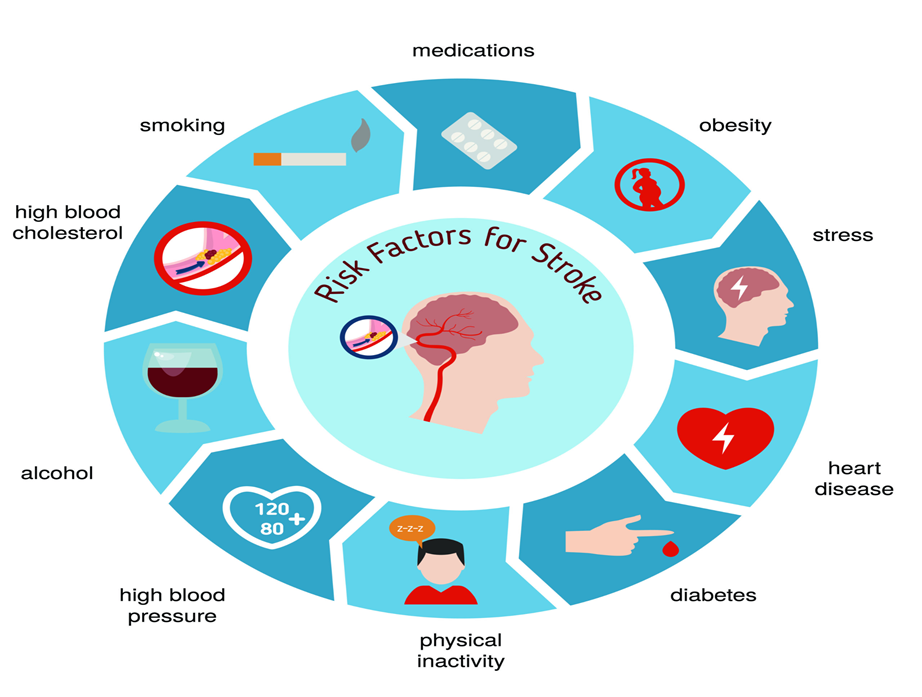
Several factors can increase the risk of stroke, and understanding them is key to prevention. Some are modifiable, meaning you can take steps to manage or reduce their impact.
Lifestyle Factors
- Smoking or tobacco use, including vaping.
- Heavy alcohol consumption.
- Recreational drug use, such as cocaine or amphetamines.
- An unhealthy diet, lack of exercise, or obesity.
Medical and Health-Related Factors
- High blood pressure (the leading cause of stroke)
- High cholesterol
- Diabetes
- Heart disease, such as coronary artery disease or heart failure.
- Atrial fibrillation or other abnormal heart rhythms.
- Sleep apnea
- Sickle cell disease
- A history of transient ischemic attack (TIA) or previous stroke
Other Contributing Factors
- Family history of stroke.
- Advancing age — the risk roughly doubles every decade after age 55.
- Gender — while men tend to have a higher overall risk, women face unique risks related to pregnancy, birth control pills, or hormone therapy.
- Race and ethnicity — Black, Hispanic, and Asian individuals often have a higher risk due to a mix of genetic and health disparity factors.
Diagnosis and Medical Evaluation
When a stroke occurs, it’s a medical emergency that demands immediate medical attention. The first thing to do is call 911 so an ambulance can arrive and take the person to the hospital quickly. During transport, an emergency worker or healthcare provider keeps a close watch on:
- Blood pressure
- Mental alertness
- Stroke symptoms like numbness, weakness, and trouble speaking, seeing, or walking.
Once in the ER (emergency room), doctors begin to figure out what type of stroke caused the problem whether it’s an ischaemic stroke (from a blocked artery) or a haemorrhagic stroke (from a burst blood vessel). Both are serious and require urgent testing to confirm the cause and begin treatment.
Diagnostic Tests and Examinations
The process usually starts with a physical exam and a neurological exam to assess:
- Reflexes and simple actions
- The nervous system and how well it’s working
- Which part of the brain was affected and how much damage occurred, imaging tests help doctors visualize the brain.
- CT scan (computed tomography): Uses X-rays to take pictures of the head, detecting bleeding, brain cell damage, or clots.
- MRI (magnetic resonance imaging): Uses a magnet and radio waves to produce detailed pictures of brain tissue, spotting tumors, plaque, or blocked arteries.
- Carotid ultrasound: Uses sound waves to view carotid arteries and check for blockage or plaque buildup.
- Transcranial Doppler (TCD): Examines artery function and identifies blocked blood flow.
Electrical and Blood Activity Tests
To evaluate electrical activity in the brain, doctors may use:
EEG (electroencephalogram): Detects seizures, confusion, or a transient ischemic attack (TIA) a mini stroke lasting less than 24 hours. It uses electrodes, wires, and a machine that records electrical signals.
To check the heart, they perform:
ECG (EKG) / Electrocardiogram: Detects atrial fibrillation, heart problems, and irregular physical activity patterns.
Blood tests also Play a key Role in Diagnosis:
Complete Blood Count (CBC): Identifies infection or anemia.
Coagulation panel/blood clotting tests: Detects clots or bleeding disorders.
Serum electrolytes: Measures the electric charge balance affecting muscle weakness, confusion, or tiredness.
Thyroid tests: Check thyroid hormone levels and detect hyperthyroidism.
Blood glucose tests: Diagnose diabetes or low blood sugar (glucose).
Cholesterol and C-reactive protein tests: Reveal high blood cholesterol, inflammation, and stroke risk.
Treatment and Management
Medical Treatment Approaches
The type of stroke ischemic stroke or hemorrhagic stroke determines the approach. In ischemic strokes, doctors often use thrombolytic or clot-busting drugs such as tissue plasminogen activator (tPA) to dissolve blood clots blocking blood vessels in the brain. If plaque, fatty deposits, or blockages are present, medicine like blood thinners, statins, or anticoagulants may be used to prevent blood clots from forming.
In severe cases, thrombectomy or surgery may be required. For hemorrhagic stroke, neurosurgeons perform procedures to stop bleeding from a ruptured aneurysm, weak spot, or break in a blood vessel. Endovascular procedures might involve placing a metal clip to seal the artery and reduce blood loss, protecting brain tissue and cells from being damaged by pressure or ruptures caused by high blood pressure or balloon-like bulges that can stretch and burst.
Rehabilitation and Recovery
Once the patient is treated, attention shifts to rehabilitation and recovery. Many survivors transition from the hospital to home, a nursing home, or a rehab center under the guidance of a health care team. Speech therapy, physical therapy, and occupational therapy help regain movement, coordination, speech, and daily activities like eating, drinking, dressing, and bathing.
During my community rotations, I witnessed how exercises and mental health support improved confidence, reducing fear, anxiety, and depression. Family, friends, and local Support groups often linked to the National Institute of Neurological Disorders and Stroke or area medical centers play a vital role in motivating patients to adjust, rebuild independence, and prevent further strokes.
Long-Term Management
Long-term management focuses on prevention by controlling underlying causes like heart disease, high blood pressure, atrial fibrillation, cholesterol, and diabetes. Doctors design a treatment plan that includes medications, diet, exercise, and healthier lifestyle habits. Following appointments, making lifestyle changes, and joining initiatives such as the Live to the Beat campaign all help lower risk over weeks, months, or even years.
Stroke Prognosis and Recovery Outlook
When experts talk about the prognosis of a stroke, they emphasize that outcomes can vary greatly from person to person. Some strokes may be fatal, while others result in permanent disabilities or long recovery periods. The survival rate depends on several factors, such as age, stroke severity, and health before the event. In my experience working with stroke patients, it’s clear that recovery rarely follows a set timeline some people recover within months, while others continue rehabilitation for years. The body’s response and the quality of treatment received play a big role in shaping the outlook.
Clinical research, such as the Framingham and Rochester stroke studies, helps provide an accurate picture of long-term outcomes. These studies showed a mortality rate of 28% at 30 days, 19% for ischemic strokes, and a 1-year survival rate of 77% for those with acute ischemic stroke. The Framingham Heart Study also found that 31% of survivors needed help caring for themselves, 20% required help with walking, and 71% faced impaired vocational capacity during long-term follow-up. Such data show that each individual’s recovery journey depends on medical factors and consistent post-stroke care.
Newer studies like the Get With The Guidelines – Stroke registry and the Austrian national stroke unit registry (2006–2017) have added more depth to understanding early mortality risk. The National Institutes of Health Stroke Scale (NIHSS) is a strong predictor of early outcomes. Researchers analyzed 77,653 cases and used multivariate analysis to find that existing heart disease, diabetes mellitus, posterior circulation stroke syndrome, and non-lacunar stroke were associated with a high risk of early stroke death. Patients with a clinical score of ≥10 had about a 35% chance of dying within 7 days of being admitted to a stroke unit.
Other complications, in clinical Pathophysiology, about 5% of uncomplicated ischemic strokes show neurologic decline due to small petechial hemorrhages or large hematomas needing evacuation. Additional factors like severe hyperglycemia, arrhythmia, and delayed reperfusion can also increase morbidity within the first 3 months.
Prevention and Healthy Living
Many strokes can be prevented by maintaining a healthy lifestyle and staying connected with your health care team. The key is to make recommendations that increase risk and to take action early rather than waiting for warning signs. Campaigns like “Live to the Beat” and “Start Small and Live Big” remind adults especially those 55 and older that even small steps like scheduling medical appointments, getting active, and eating healthy can lead to big results over time.
A few prevention steps that consistently show results include:
1. Choosing healthy foods and drinks – Focus on fresh fruits, vegetables, and meals low in saturated fats, trans fat, and cholesterol. Add high-fiber foods, and limit salt (sodium) to help lower blood pressure and improve your diet. I always tell patients to check CDC nutrition resources for tips and healthy choices that fit their lifestyle.
2. Adopt a heart-healthy diet (DASH/Mediterranean)
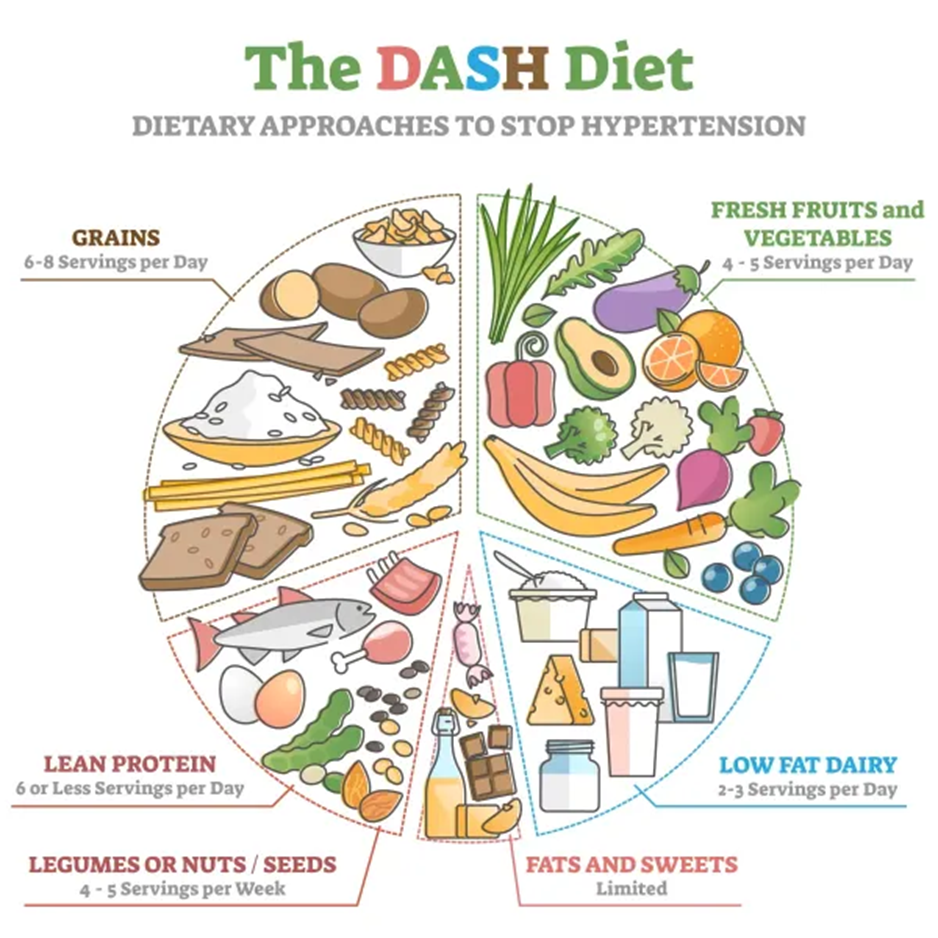
3. Keeping a healthy weight – Excess body fat and obesity can increase stroke risk. Regularly checking your body mass index (BMI) using the CDC BMI calculator or through your doctor can help you stay within a healthy range. Tracking your waist and hip measurements also gives insight into your health.
4. Getting regular physical activity – The Surgeon General recommends at least 2 hours and 30 minutes of moderate-intensity aerobic exercise each week (like a brisk walk). Children and teens should get 1 hour every day. Exercise helps lower cholesterol, control blood pressure, and keep you strong enough to enjoy daily life.
It’s also vital to make conscious choices about habits that affect your blood pressure and cholesterol:
- Don’t smoke – Cigarette smoking increases your chances of having a stroke. If you smoke, seek help from your doctor or use CDC quitting resources.
- Limit alcohol – Avoid drinking too much alcohol; men should have no more than two drinks per day, and women no more than one.
- Control your medical conditions – Manage heart disease, diabetes, and high cholesterol through regular check-ups and medicine when prescribed. Check cholesterol every five years, and control blood pressure with lifestyle changes, low-sodium foods, or prescribed medicine.
- Take your medicine and follow your doctor’s instructions closely. Never stop a treatment plan without talking to your pharmacist or doctor.
Conclusion
Life after a stroke is a journey of strength, patience, and determination. Recovery takes time, but with consistent rehabilitation, emotional support, and medical guidance, survivors can regain independence and improve their quality of life. Caregivers and loved ones play a vital role in motivation and daily recovery efforts. Staying alert to warning signs, following treatment plans, and maintaining regular follow-ups with healthcare providers help prevent future complications. With perseverance and support, every survivor can move forward toward a healthier, more fulfilling life.
FAQ’s
What should I do if I think someone is having a stroke?
Call 911 immediately. Recognize stroke symptoms, act fast, and get emergency care to reduce severe complications and fatal outcomes.
Can a stroke be prevented?
Yes, through healthy lifestyle choices, controlling blood pressure, cholesterol, avoiding smoking, exercising regularly, and following your health care team’s advice.
Can i live a normal life after a stroke?
Many stroke survivors can thrive with rehabilitation, support, and lifestyle changes. Developing new routines and adjusting habits helps regain independence.
How can family members help a stroke survivor?
Caregivers, family members, and friends can help comply with the prevention plan, attend therapy appointments, and provide emotional support during recovery.

 Medically reviewed by
Medically reviewed by