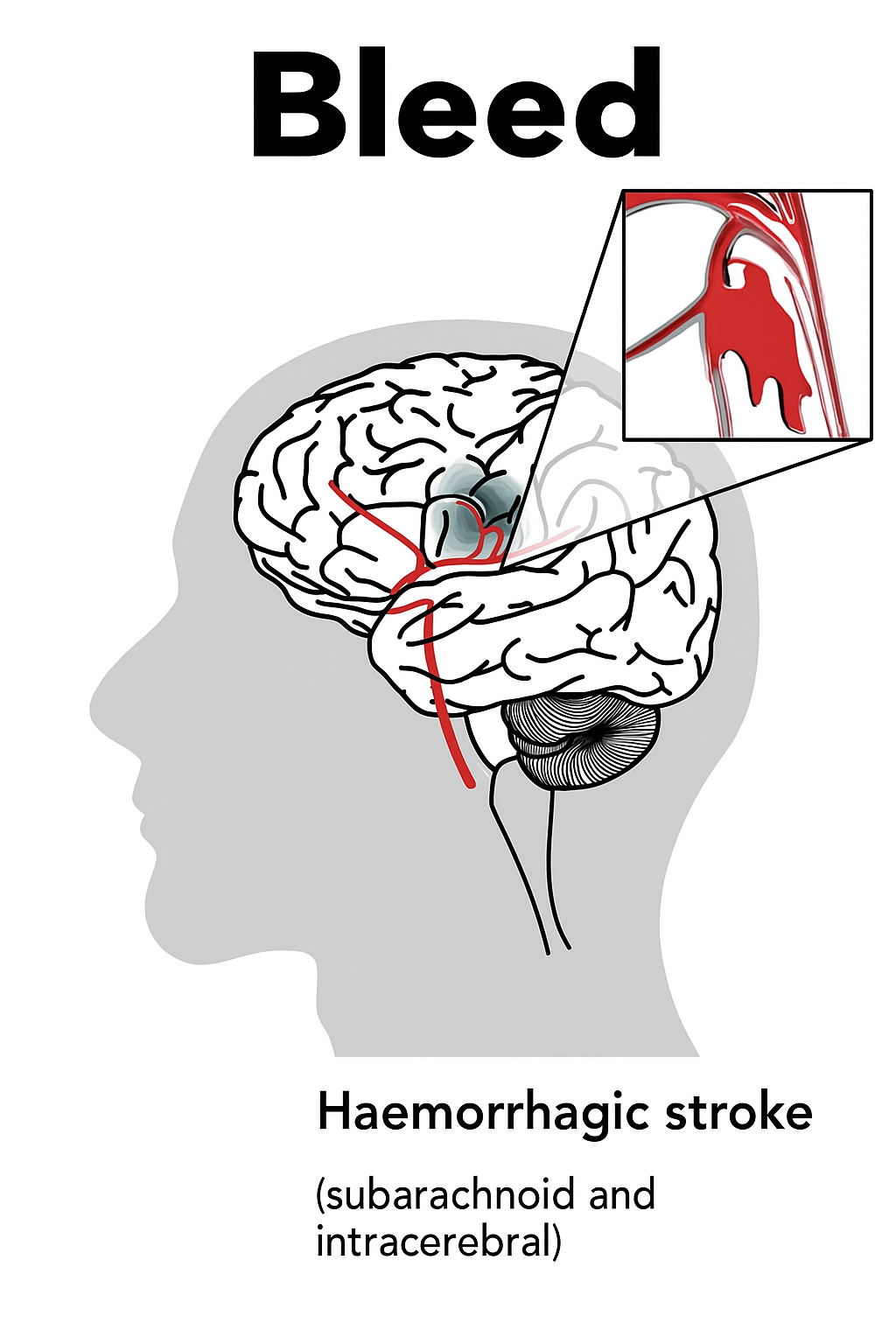
What Happens During a Haemorrhagic Stroke?
The Science Behind the Bleed
A haemorrhagic stroke occurs when a weakened blood vessel ruptures, causing blood to leak either within the brain tissue (intracerebral) or into the space surrounding the brain (subarachnoid). This bleeding exerts direct pressure on brain structures, triggering what physicians call a mass effect. As intracranial pressure rises, oxygen delivery falls, leading to direct tissue toxicity where brain cells are damaged by both pressure and chemical injury.
This chain reaction unfolds in two phases:
Primary injury
Immediate compression from the hematoma causes sudden neurological deficits such as weakness or confusion.
Secondary injury
Hours later, inflammation, oxidative stress, and iron toxicity from blood breakdown worsen brain swelling and damage. (Frontiers in Neurology, 2023)
Types of Haemorrhagic Stroke
Intracerebral Haemorrhage (ICH)
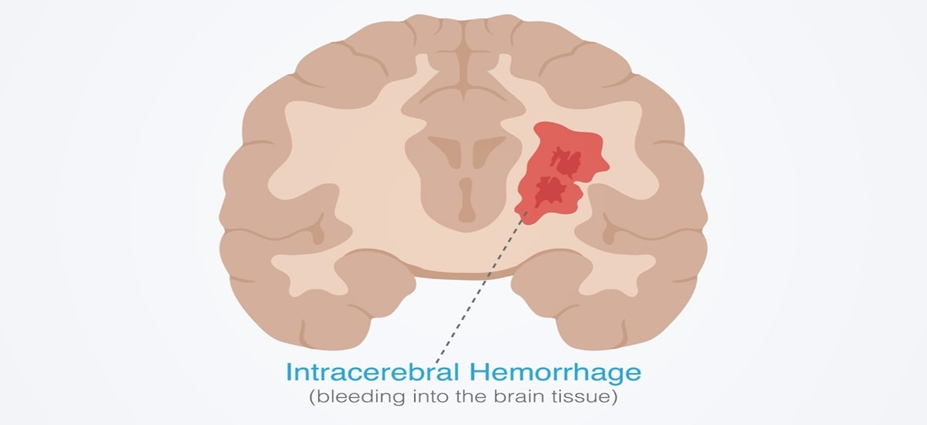
ICH involves bleeding within the brain’s functional tissue commonly affecting the basal ganglia, thalamus, pons, or cerebellum. Chronic hypertension and small vessel disease are leading causes (PubMed Central, 2025). These fragile vessels rupture under sustained pressure, especially in older adults or those with diabetes.
Subarachnoid Haemorrhage (SAH)
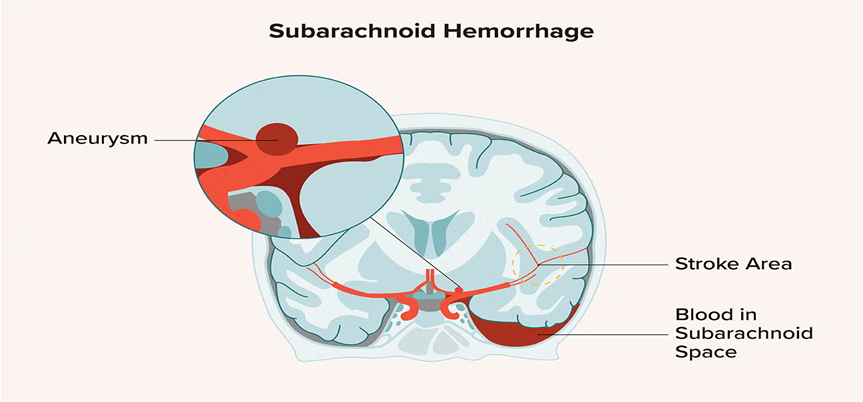
SAH occurs when bleeding enters the subarachnoid space, often from a ruptured saccular (berry) aneurysm. The result is a sudden spike in intracranial pressure and a severe, “worst headache of my life” presentation (NCBI, 2024). SAH requires rapid imaging and urgent aneurysm repair either surgical clipping or endovascular coiling to prevent re-bleeding and death.
Global Burden of Haemorrhagic Stroke
Haemorrhagic stroke remains profound because of its high fatality rate and the severe long-term disabilities it often causes.
According to Global heart it represents only 10% to 27% of all stroke cases, it is responsible for a disproportionately higher share of stroke-related deaths and the 30-day mortality rate particularly for intracerebral haemorrhage can exceed 50%, underscoring its critical severity.
Causes and Risk Factors
Haemorrhagic strokes arise from a mix of vascular fragility, chronic disease, medication use, and lifestyle factors.
Uncontrolled Hypertension: The single most significant modifiable cause; persistent high blood pressure weakens small arteries, making rupture more likely.
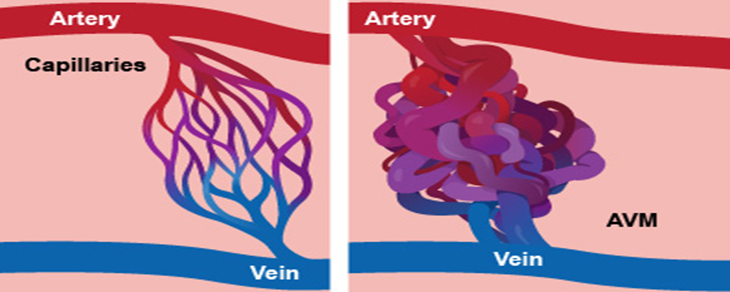
Aneurysms and AVMs: Structural defects like aneurysms and arteriovenous malformations increase risk of rupture, particularly in younger individuals. (JamaNetwork, 2023)
Anticoagulant Therapy: Overuse or mismanagement of blood thinners raises bleeding risk; immediate reversal of anticoagulation is crucial in emergencies. (StatPearls, 2024).
Trauma and Lifestyle Triggers: Head injuries, heavy alcohol use, smoking, and stimulant drugs like cocaine can precipitate bleeding events. (WHO, 2024)
Signs and Symptoms
Haemorrhagic stroke usually begins suddenly, with weakness or numbness on one side, speech trouble, vision loss, vomiting, or confusion. Unlike ischemic stroke, symptoms of haemorrhagic stroke often progress rapidly within minutes as bleeding expands.(Medscape, 2024)
In Subarachnoid Haemorrhage, the hallmark sign is a sudden, explosive headache often followed by neck stiffness, photophobia, vomiting, or loss of consciousness. According to NCBI (2023), immediate evaluation is critical since early detection can prevent re-bleeding and fatal outcomes.
Diagnosis and Emergency Response
Imaging and Tests
The non-contrast CT scan remains the fastest and most reliable diagnostic tool for detecting intracranial bleeding. When vascular abnormalities are suspected, CT angiography (CTA) or digital subtraction angiography (DSA) is used for detailed visualization. (ScienceDirect, 2024)
MRI provides added sensitivity in later stages but is not first-line in emergencies.
Importance of Timely Response
Speed is crucial MDPI Journals (2024) report that hematoma expansion within the first few hours is a major determinant of poor outcome. Prompt hospital transfer allows for blood pressure control, anticoagulant reversal, and early surgical evaluation dramatically improving survival rates.
Treatment and Acute Management
Immediate Stabilization and BP Control
The first priority is maintaining airway, breathing, and circulation. Tight blood pressure management (<140 mmHg systolic in select patients) limits further bleeding (PMC, 2024). Rapid reversal of anticoagulation and control of intracranial pressure through medical or mechanical methods are also key steps.
Surgical and Interventional Care
Large or life-threatening bleeds may require hematoma evacuation, while SAH often demands aneurysm repair via clipping or coiling. Early intervention prevents re-bleeding and neurological decline (American Heart Association, 2023).
ICU and Post-Surgical Management
After stabilization, patients need close monitoring in neuro-ICU settings for complications such as vasospasm, seizures, infections, and electrolyte imbalance (Nature Communications, 2024). A coordinated team approach ensures comprehensive care.
Rehabilitation and Recovery
Recovery focuses on regaining function, independence, and psychological resilience.
- Physical and Speech Therapy: Early, structured rehabilitation improves movement, coordination, and speech outcomes. (PubMed, 2024)
- Psychological Support: Emotional effects like depression or anxiety are common counselling and peer support play a vital role in recovery.
- Lifestyle Adjustment: Strict blood pressure control, smoking cessation, and healthy living reduce recurrence risk. (Canadian Stroke Best Practices, 2024)
Prevention and Risk Reduction
Preventing haemorrhagic stroke revolves around consistent risk factor management and healthy habits.

- Managing Hypertension and Comorbidities: Keeping blood pressure within target range remains the most effective preventive strategy. (AHA Journals, 2025)
- Healthy Lifestyle Habits: Regular exercise, reduced alcohol, and a low-salt diet support vascular health.
- Medication Adherence and Follow-Ups: Continuous medical monitoring and adherence to prescribed drugs prevent recurrence. (Canadian Stroke Best Practices, 2020)
- Weight and Cholesterol Management: Maintaining a healthy body weight and controlling lipid levels reduce overall vascular strain and prevent small-vessel damage that can lead to intracerebral bleeding.
- Stress Reduction and Mental Health Support: Chronic psychological stress contributes to high blood pressure and inflammation; relaxation techniques, counseling, and mindfulness reduce stroke risk.
Real-Life Perspective — Why Awareness Saves Lives?
At 48, Maria never expected a sudden, excruciating headache to change her life. She described it as “the worst pain I’ve ever felt like something burst inside my head.” Within minutes, she became dizzy, disoriented, and began vomiting.
Recognizing that these weren’t typical migraine symptoms, her husband immediately called emergency services. At the hospital, a CT scan confirmed a haemorrhagic stroke bleeding from a ruptured artery in her brain. Quick diagnosis allowed doctors to perform emergency surgery to relieve pressure and prevent further brain damage.
Maria spent several weeks in the intensive care unit, followed by months of physical and speech therapy. The recovery was slow, but her timely treatment made all the difference she regained her mobility and independence.
Her story highlights a crucial message: knowing the warning signs and acting fast can save a life. Haemorrhagic strokes progress rapidly, but early recognition and immediate medical care can prevent permanent disability or death.
Conclusion
Haemorrhagic stroke is less common but far more deadly than ischemic stroke. It’s primarily linked to uncontrolled hypertension and vascular malformations. Early recognition, accurate imaging, and treatment in specialized centers are the cornerstones of better outcomes. Monitor your blood pressure, act fast on neurological symptoms, and stay consistent with healthy habits. Small daily choices like reducing salt and quitting smoking can prevent catastrophic bleeding events. Awareness isn’t optional it’s lifesaving.

 Medically reviewed by
Medically reviewed by