Endometriosis is a persistent gynaecological disorder which affects millions of females globally at times when they are in their reproductive age. Although it is highly prevalent, it is not sufficiently diagnosed and understood. Endometriosis is categorised into four stages: Stage 1 (minimal), Stage 2 (mild), Stage 3 (moderate), and Stage 4 (severe), based on the location, depth, extent of endometrial implants, and presence of adhesions or ovarian cysts.
Stage 2 endometriosis, or mild endometriosis as it is also called, may not be that severe, but it can be quite painful, leading to menstrual difficulties and fertility problems. This paper gives an in-depth description of stage 2 endometriosis, its symptoms, causes, diagnosis, treatment choices, and lifestyle management strategies of the condition.
What is Stage 2 Endometriosis?
Superficial endometrial implants, which are more abundant and a little deeper than those which occur in stage 1, characterise stage 2 endometriosis. These lesions typically occur in the pelvic area, including the ovaries, fallopian tubes, pelvic lining (peritoneum), and uterine supporting ligaments.
Stage 2 endometriosis is typically not accompanied by large adhesions or damage to internal organs, as opposed to advanced stages, but even the inflammatory reaction to the lesions may cause serious discomfort and quality-of-life problems. One should know that the endometriosis stage is not always associated with the intensity of pain. Women with stage 2 disease can have very strong symptoms, and those who develop the disease in the advanced stages may be suffering very little. Stage 2 endometriosis has symptoms which differ with individuals. Whereas a few people might experience mild symptoms, others might go through debilitating pain that disrupts normal day-to-day practices. The most frequent symptom is chronic pelvic pain. It can be permanent or periodical, and in most cases, it gets worse before or during the menstrual period.
Causes and Risk Factors
Endometriosis remains an enigma about the precise cause, but some of the theories and risk factors linked to the condition exist.
Possible Causes
Retrograde menstruation, menstrual blood flows backwards into the pelvic cavity. Imbalanced functioning of the immune system, which makes the endometrial tissue implant in an extrauterine position. Hormonal imbalance, especially excess estrogen.
- Genetic predisposition.
- Inflammatory reaction, which facilitates the progression of lesions.
- Early onset of menstruation.
- Short menstrual cycles.
- Heavy or prolonged periods.
- Endometrial family history.
- Late childbearing or infertility.
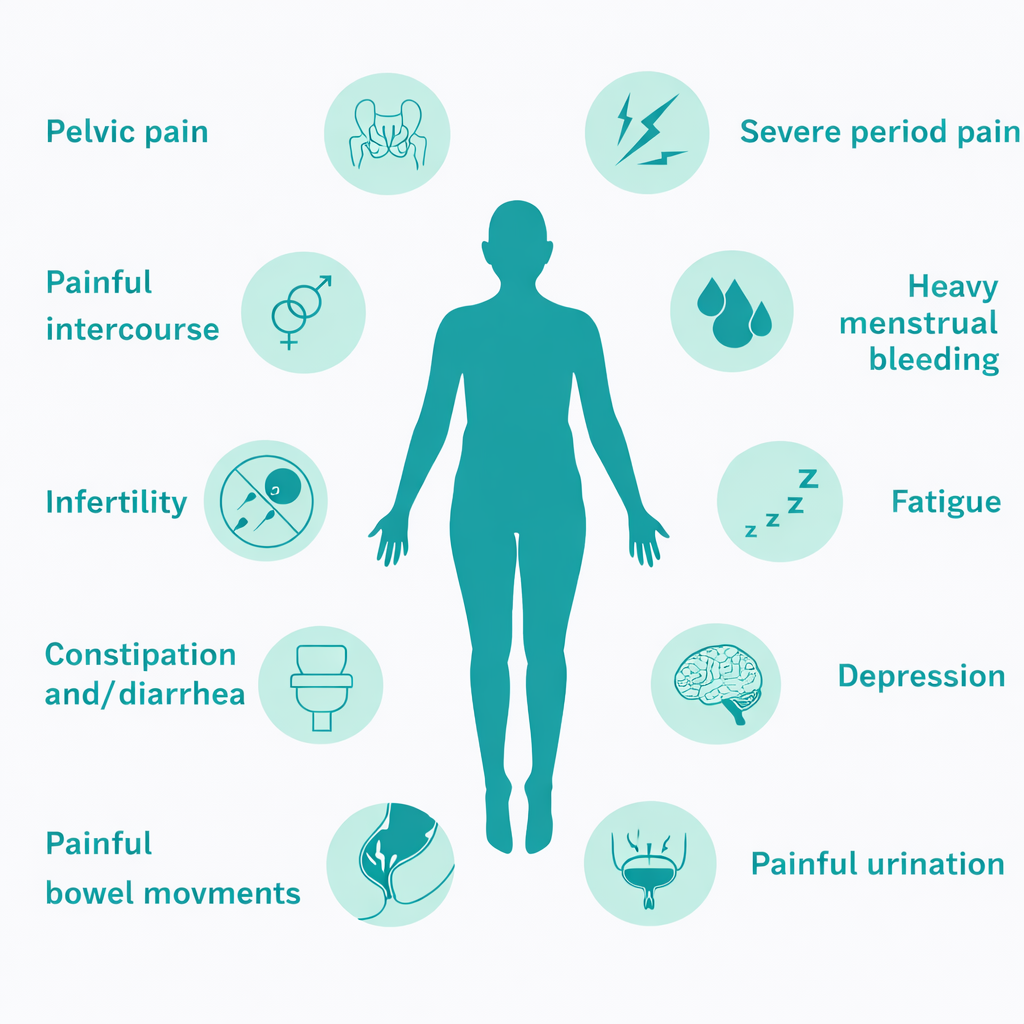
Symptoms of Stage 2 Endometriosis (Moderate Endometriosis)
- Pelvic pain: Persistent or recurring pain in the lower abdomen or pelvis, often worsening before and during menstruation.
- Painful periods (dysmenorrhea): Menstrual cramps that are more intense, longer-lasting, and may not respond well to standard pain relievers.
- Pain during or after intercourse (dyspareunia): Deep pelvic pain during sex is common due to lesions near the uterosacral ligaments or pelvic organs.
- Lower back and abdominal pain: Pain may radiate to the lower back or thighs.
- Heavy or irregular menstrual bleeding: Includes menorrhagia (heavy periods) or spotting between cycles.
- Gastrointestinal symptoms: Bloating, constipation, diarrhea, nausea, or pain during bowel movements, especially around menstruation.
- Urinary discomfort: Painful urination or urgency, particularly during periods, if lesions are near the bladder.
- Fatigue: Chronic pain and inflammation often lead to ongoing tiredness and reduced energy levels.
- Fertility challenges: Stage 2 endometriosis can interfere with ovulation, egg quality, or implantation, making conception more difficult for some women.
What is the Diagnosis of Stage 2 Endometriosis?
The diagnosis of endometriosis may be complicated and sometimes takes many years to be diagnosed because of similar symptoms with other diseases.
1. The Physical Examination and Medical History
The detailed history of menstrual history and pain is necessary. A pelvic examination can show tenderness or nodules, but stage 2 lesions are not easily observed through the hands.
2. Imaging Tests
Ultrasound is useful in determining ovarian cysts, but it might fail to detect the small implants. Pelvic structures can be assessed by MRI in a limited number of instances.
3. Laparoscopy (Gold Standard)
Diagnosis of endometriosis is best done through laparoscopic surgery. In the process, a surgeon can visually determine lesions as well as give them a stage depending on their size, level of depth or location. A biopsy can be carried out to confirm.
Medical Treatment of Stage 2 Endometriosis
Endometriosis has no treatment, but the symptoms can be effectively treated using a combination of medical, surgical, and lifestyle interventions.
1. Pain Management
Nonsteroidal anti-inflammatory drugs (NSAIDs), including ibuprofen or naproxen.
2. Hormonal Therapy
Hormonal therapy is done to lower estrogen levels and inhibit lesion development:
- Oral contraceptive pills in combination.
- Progestin-only therapy
- Hormonal IUDs
- GnRH agonist or antagonist (selectively used, as it also has side effects).
3. Surgical Treatment
Lesions might be excised or ablated laparoscopically in the case of persistent pain following medical therapy or in the case of fertility issues. With the help of surgery, it is possible to alleviate pain greatly and enhance the results of reproductive activities.
4. Fertility Treatment
Women having difficulties with conception can be helped with:
- Ovulation induction
- Intrauterine insemination (IUI)
- In vitro fertilisation (IVF), which is a factor of the factors.
Lifestyle and Dietary Management
The role of lifestyle changes in the control of symptoms and the overall well-being is significant.
Anti-Inflammatory Diet
- Eat more fruits, vegetables, whole grains and omega-3 fatty acids.
- Restrict processed foods, red meat, sugar, and trans fats.
- Minimise alcohol and caffeine consumption.
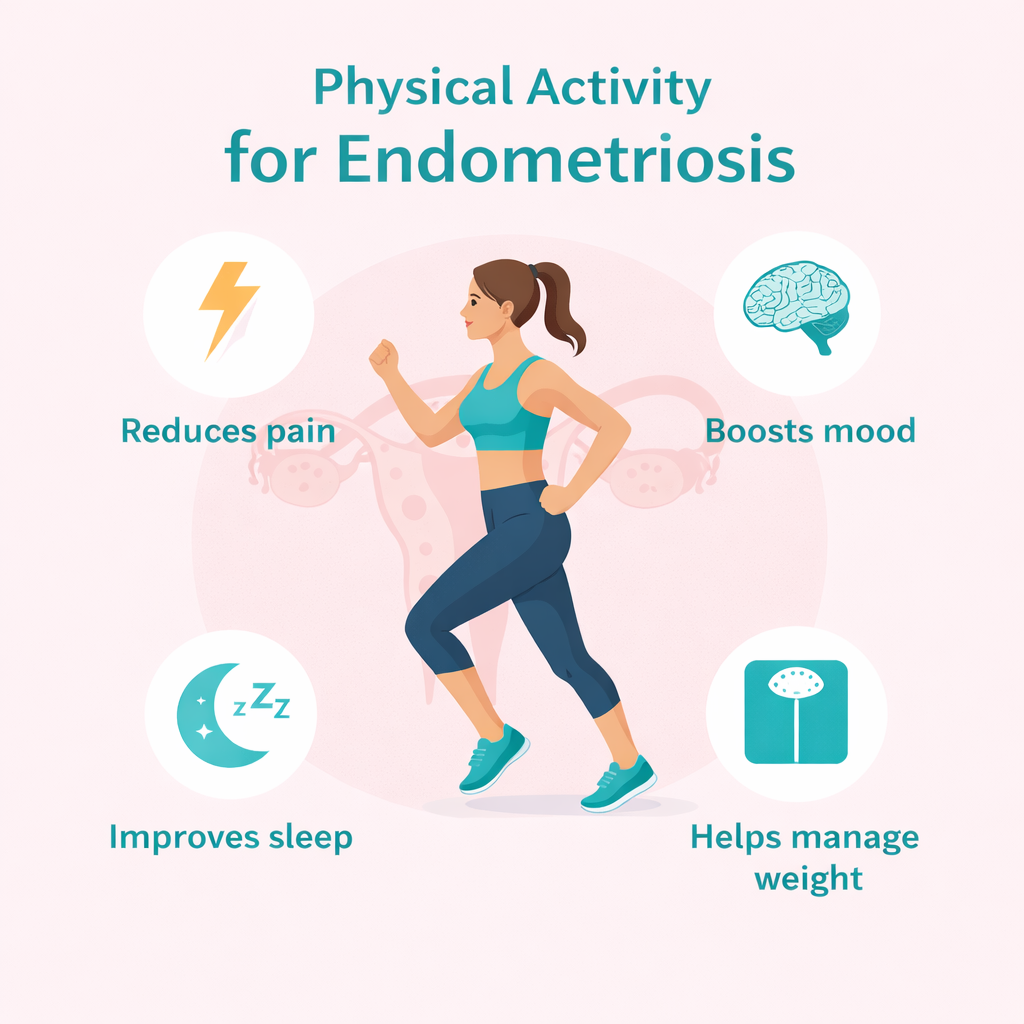
Physical Activity
Pain reduction and better circulation can be achieved through gentle exercises like walking, yoga and stretching.
Stress Management
Symptoms may be aggravated by chronic stress. Meditation, mindfulness, and deep breathing exercises, as well as counselling, can be helpful.
Sleep and Rest
Sleep is essential to the immune system and hormonal balance. Employing Imagery: Emotional and Psychological Effects
Stage 2 endometriosis is emotionally burdensome. It is possible that chronic pain, infertility, and late diagnosis can lead to anxiety, depression, and isolation.
In search of emotional support with:
- Counselling or therapy
- Support groups
- Free interaction with medical professionals and family can contribute to a substantial increase in mental health and coping capacity.
Is Stage 2 Endometriosis Progression Possible?
Yes, endometriosis may advance with time in its untreated state, but the progression of endometriosis is not predictable. Other women stay stable over several years, whereas some could progress to stage 3 or 4. Diagnosis and proactive intervention may prevent or delay the progression and maintain the quality of life.
Living Well
The diagnosis of stage 2 endometriosis is not the future. When women receive the appropriate treatment plan, lifestyle adjustments, and support, they are able to live active and fulfilling lives. One-on-one treatment is necessary since the symptoms and treatment reactions are diverse.
Conclusion
A mild yet effective type of chronic condition, Stage 2 endometriosis is the type that should be considered in time and treated properly. Although it might not be accompanied by such critical damage to the anatomy, the symptoms can have a severe impact on the physical, emotional, and reproductive health. Knowledge of the condition, research on treatment and adoption of supportive lifestyle skills will enable the women to be more empowered to control their health and enhance their quality of life.
FAQ’s
1. What is stage 2 endometriosis?
Mild endometriosis is stage 2 endometriosis, which presents itself in the form of multiple superficial endometrial lesions outside the uterus. They can be a little more profound and extensive than stage 1 but, as a rule, do not include big adhesions and organ damage.
2. Is the stage 2 endometriosis severe?
Even though considered mild, stage 2 endometriosis may still be very painful and lead to menstrual issues and fertility problems. The stage of the disease is not always associated with the severity of its symptoms.
3. What are the symptoms of stage 2 endometriosis?
The symptoms are painful periods, persistent pain in the pelvis, pain during or after intercourse, bloating, bowel discomfort, menstruation, lower back pain, tiredness, and difficulty in conceiving in some instances.
4. Is stage 2 endometriosis capable of resulting in infertility?
Yes, stage 2 endometriosis may interfere with fertility, but most women with this stage naturally conceive. Ovulation or implantation may be hampered by inflammation, hormonal imbalance or slight scarring of the pelvis.
5. Should stage 2 endometriosis be surgically treated?
Surgery is not necessarily a necessity. It can be advised when the pain is not improved by use of medication or where fertility problems continue. The choice of treatment is based upon symptoms, age, and reproductive objectives.
6. What does lifestyle intervention contribute to the management of stage 2 endometriosis?
Symptoms can be treated and overall well-being can be improved with the help of an anti-inflammatory diet, regular mild physical activities, reduction of stress, enough sleep, elimination of smoking and excessive drinking of caffeine.
7. Does pregnancy ameliorate stage 2 endometriosis?
Hormonal changes and pregnancy conditions are temporarily effective in the symptoms, but pregnancy is not a cure. Symptoms can come back following delivery or when their normal menstrual cycles come back.
8. When should I see a doctor?
A medical professional needs to be approached if you are experiencing intense menstrual pain, pain in the pelvis which is disruptive to normal life, painful sex or pregnancy problems.

 Medically reviewed by
Medically reviewed by