High cholesterol is one of the leading risk factors for heart disease, yet many people remain unaware of how silently it can damage the body. When excess cholesterol circulates in the blood, it begins to form plaque inside the arteries, a process known as atherosclerosis. Over time, this buildup can narrow blood vessels, limit oxygen supply, and trigger serious conditions such as stroke or heart attack. The good news is that with the right combination of diet, exercise, and medical care, cholesterol levels can be controlled. Understanding its causes, prevention methods, and treatment options is the first step toward a healthier heart.
What is High Cholesterol and Why Does it Matter?
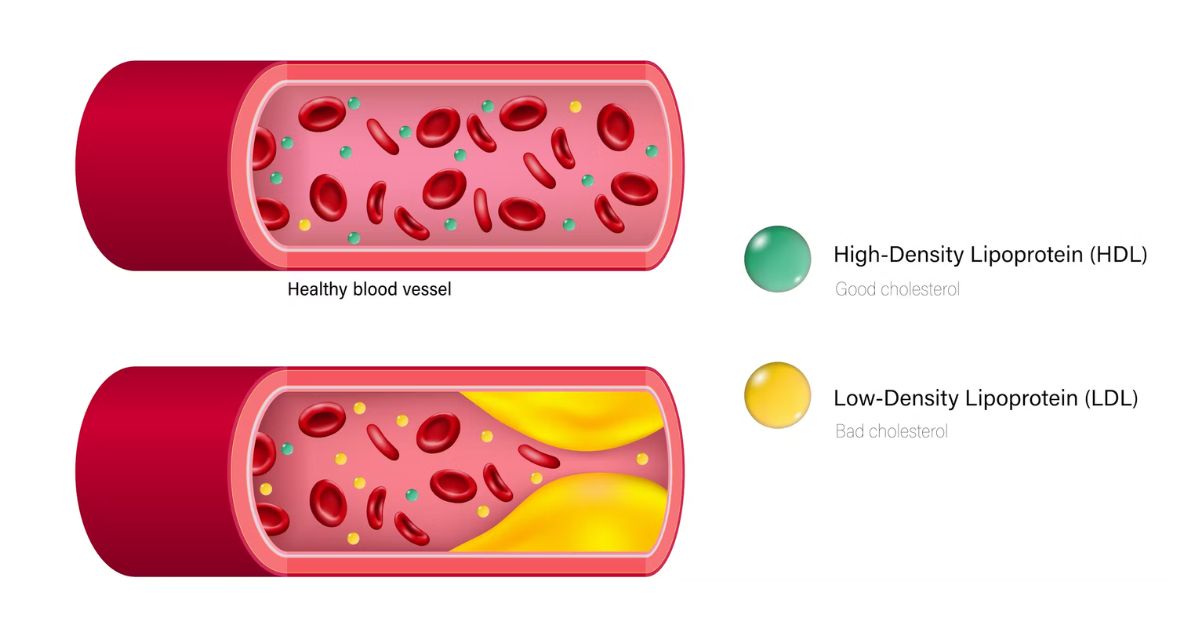
Cholesterol is a type of fat (lipid) found in your blood. While it is essential for building healthy cells, too much cholesterol can be harmful. The problem begins when cholesterol builds up in the walls of your arteries, forming plaque. Over time, this process leads to atherosclerosis, which is a hardening and narrowing of the arteries.
Good Cholesterol (HDL) vs. Bad Cholesterol (LDL)
There are different types of cholesterol:
- LDL (Low-Density Lipoprotein): Often called “bad cholesterol,” LDL carries cholesterol to your arteries. High levels of LDL are directly linked to plaque buildup and blockages.
- HDL (High-Density Lipoprotein): Known as “good cholesterol,” HDL helps remove excess cholesterol from the bloodstream and carries it back to the liver for disposal. Higher levels of HDL are protective for heart health.
- VLDL (Very Low-Density Lipoprotein): VLDL is rich in triglycerides, another type of fat in the blood, and contributes to plaque buildup.
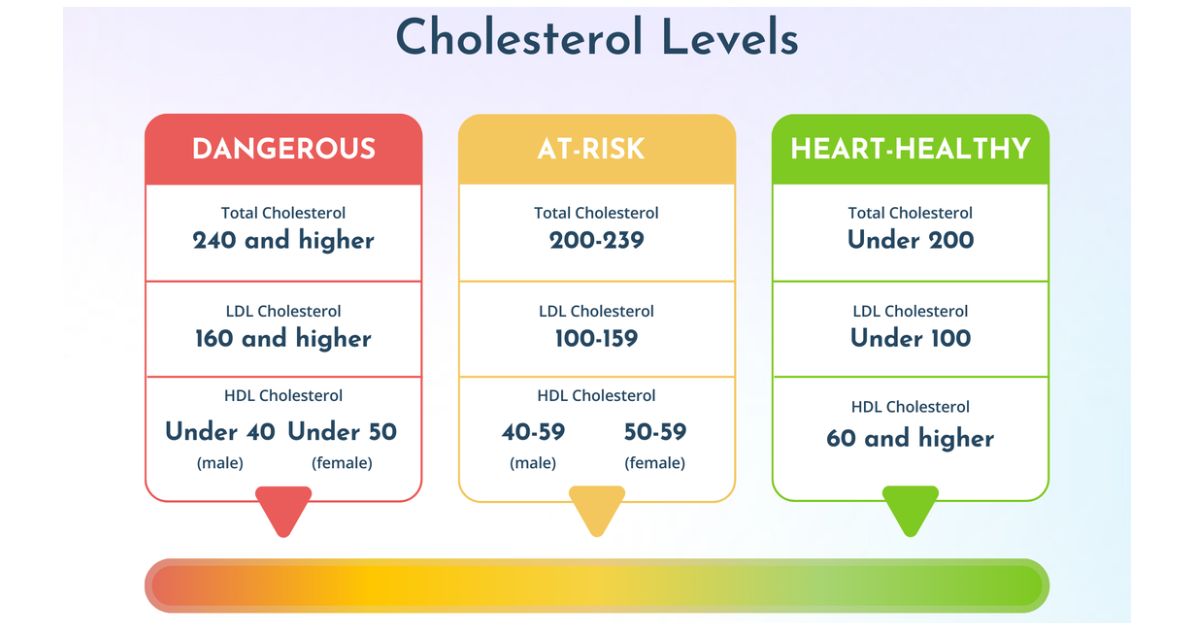
In the U.S., about 93 million adults have high total cholesterol levels (≥200 mg/dL), and nearly 29 million have dangerously high LDL cholesterol (≥160 mg/dL). This imbalance increases the risk of artery blockage and serious cardiovascular diseases.
What Happens When Cholesterol Levels Get Too High?
When LDL remains elevated, it penetrates the walls of the arteries and damages the endothelium (the inner lining of blood vessels). This triggers an inflammatory response where immune cells try to “digest” the cholesterol but end up forming fatty deposits. Over time, these deposits turn into hard plaque due to calcification and fibrosis. Plaque narrows the arteries, reduces oxygen supply, and can eventually rupture, leading to heart attack, angina, or stroke.
Causes of High Cholesterol and Arterial Plaque
High cholesterol and arterial plaque buildup usually result from a combination of genetics, underlying medical conditions, and lifestyle choices. Cholesterol plays an important role in the body, but when LDL levels rise too high, fatty deposits begin to accumulate in artery walls, narrowing them and restricting blood flow. Over time, this can lead to atherosclerosis, heart attack, or stroke. While lifestyle factors such as unhealthy diets and lack of exercise are the leading contributors, medical conditions and inherited disorders also play a significant role. Understanding these causes helps in both prevention and early treatment of heart disease.
Genetic, Medical, and Lifestyle Factors Behind Cholesterol Problems
Some individuals are predisposed to high cholesterol due to genetic disorders. One of the most well-known conditions is Familial Hypercholesterolemia (FH), which affects about 1 in 250 Americans. People with FH often have mutations in genes like ApoB, LDLR, or PCSK9, resulting in extremely high LDL levels regardless of their diet or lifestyle. Left untreated, FH can cause premature heart disease and heart attacks, sometimes as early as in the 30s or 40s.
Certain medical conditions also raise cholesterol:
- Diabetes alters lipoprotein metabolism, raising triglycerides and LDL.
- Hypothyroidism reduces the body’s ability to clear LDL from the blood.
- Kidney disease and liver disorders interfere with cholesterol production and balance, leading to abnormal lipid profiles.
However, in most cases, high cholesterol is linked to lifestyle habits. Diets high in saturated fats, trans fats, and refined sugars increase LDL and triglycerides. Lack of physical activity reduces levels of HDL, the “good” cholesterol that helps clear fatty deposits. Obesity not only raises LDL but also creates chronic inflammation that accelerates plaque buildup. Smoking is another major factor, studies from the American Heart Association (AHA) show that smokers are 2–4 times more likely to develop coronary artery disease (CAD) compared to non-smokers.
Ultimately, high cholesterol is often the result of a combined effect: genetics may create a predisposition, while lifestyle habits accelerate the damage. Recognizing these risk factors is the first step toward prevention and treatment.
Common Symptoms and Warning Signs to Watch For
Silent Signs of High Cholesterol You Might Miss
High cholesterol is often called a “silent killer” because it usually has no symptoms until advanced complications occur. However, warning signs of plaque buildup may include:
- Chest pain or angina
- Shortness of breath during exertion
- Fatigue and weakness
- Numbness in arms or legs (linked to PAD)
When to See a Doctor for Cholesterol Testing
The American Heart Association recommends that adults over age 20 should get checked every 4–6 years, while those with risk factors such as obesity, diabetes, or family history should test more often. A blood test (lipid panel) measures LDL, HDL, total cholesterol, and triglycerides.
Risk Factors That Increase Your Chances of Atherosclerosis
Age, Gender, and Family History Risks
As people age, cholesterol tends to rise naturally due to slower metabolism and vascular changes. Men are at a higher risk than women before age 55, but after menopause, women’s risk increases significantly. A family history of early heart disease (before 55 in men or 65 in women) also increases the likelihood of atherosclerosis.
How Obesity, Smoking, and Diet Raise Your Risk?
Obesity raises triglycerides and LDL levels while lowering HDL. Poor diets high in processed foods and sugar accelerate artery plaque buildup. Smoking damages the endothelium and increases oxidized LDL (OxLDL), which is more likely to stick to artery walls and form plaques.
How High Cholesterol Affects Your Heart and Blood Vessels
Cholesterol and Coronary Artery Disease (CAD)
High cholesterol is the leading cause of coronary artery disease (CAD), which occurs when plaque narrows the coronary arteries that supply blood to the heart. CAD affects about 20.1 million adults in the U.S., making it the most common type of heart disease.
The Link Between Cholesterol and Stroke
Plaque buildup in carotid arteries reduces blood supply to the brain and may rupture, causing a clot. This can lead to an ischemic stroke, the most common type of stroke in the U.S. According to the CDC, nearly 800,000 Americans experience a stroke each year, and high cholesterol is one of the top risk factors.
Diagnosis and Tests for Detecting High Cholesterol
Blood Tests for Measuring Cholesterol Levels
- A lipid panel checks:
- Total cholesterol
- LDL
- HDL
- Triglycerides
Healthy ranges (mg/dL):
| Type of Cholesterol | Healthy Range | Borderline High | High Risk |
| Total | <200 | 200–239 | ≥240 |
| LDL (Bad) | <100 | 130–159 | ≥160 |
| HDL (Good) | ≥60 | 40–59 | <40 |
| Triglycerides | <150 | 150–199 | ≥200 |
Treatment Options: Medications, Lifestyle, and Procedures
Managing plaque buildup in arteries and high cholesterol involves a combination of medications, lifestyle changes, and medical procedures, depending on the severity of the condition. For patients with mild to moderate issues, lifestyle modifications such as eating a diet low in saturated fat, exercising regularly, and quitting smoking can significantly lower cardiovascular risk. However, when lifestyle measures are not enough, doctors often recommend medications to reduce LDL cholesterol and stabilize plaques. For advanced cases where arteries are severely narrowed or blocked, medical procedures are necessary to restore blood flow and prevent heart attacks or strokes. Treatment is usually personalized, and doctors often combine different strategies to achieve the best results for long-term heart health.
Statins, Other Drugs, and Medical Procedures for Blocked Arteries
Statins are the cornerstone of cholesterol management. They not only lower LDL but also stabilize arterial plaques, reducing the risk of rupture. Research shows that statins can lower the chance of heart attack and stroke by 25–30%. Other effective medications include ezetimibe, which reduces cholesterol absorption from food; PCSK9 inhibitors, powerful injectable drugs that can lower LDL by up to 60%; and bile acid sequestrants, which bind bile acids in the intestine to help remove cholesterol from the body.
For patients with severe blockages, medications alone may not be enough. In such cases, doctors recommend interventional procedures:
- Angioplasty: A small balloon is inserted and inflated to widen narrowed arteries, restoring blood flow.
- Stent placement: Often done after angioplasty, a wire mesh tube is left inside the artery to keep it open and reduce the risk of re-narrowing.
- Bypass surgery: A vein or artery from another part of the body is used to reroute blood around the blockage, allowing blood to reach the heart muscle.
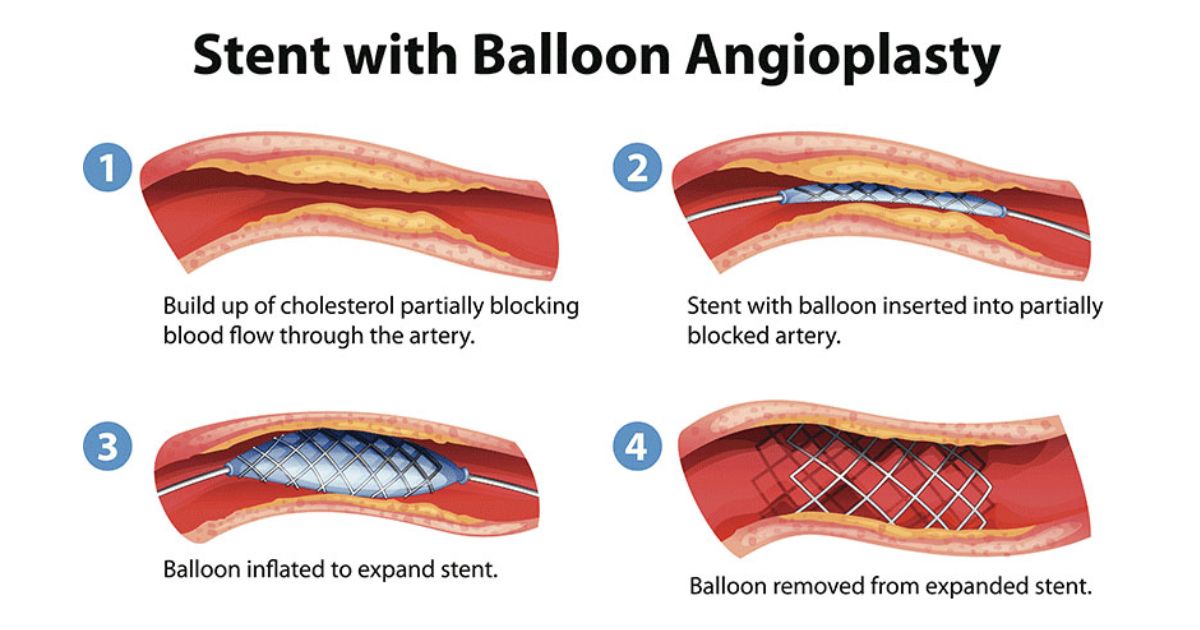
These procedures are usually reserved for patients with severe coronary artery disease (CAD), angina, or those at high risk of heart attack. Advances in minimally invasive techniques have made angioplasty and stent placement safer and more effective, often requiring shorter hospital stays and recovery times compared to traditional bypass surgery.
Together, medications, lifestyle changes, and procedures form a powerful, multi-layered approach to managing plaque buildup and protecting long-term cardiovascular health.
Can Plaque Buildup in Arteries Be Reduced or Reversed?
Plaque buildup in arteries, called atherosclerosis, is a leading cause of heart disease, stroke, and peripheral artery disease (PAD). It occurs when fats, calcium, and inflammatory cells accumulate inside the arterial walls, causing them to narrow and harden. This reduces blood flow, increases blood pressure, and raises the risk of sudden blockages that can trigger heart attacks or strokes.
For many years, doctors believed that once plaque formed, it could not be reduced. However, modern research shows that while complete reversal of advanced plaque is difficult, it can be slowed, stabilized, and in some cases even partially reduced. The key lies in combining lifestyle changes with medical therapies. A diet rich in whole grains, vegetables, fruits, nuts, and healthy fats (such as omega-3s) lowers LDL and raises HDL, which protects the arteries. Regular exercise improves circulation and helps prevent plaque from growing further. Quitting smoking and maintaining a healthy weight also reduce inflammation and stress on arteries. Together, these measures create conditions where plaque can stop progressing and even regress slightly in some patients.
Lifestyle Changes and Emerging Research on Reversing Atherosclerosis
Lifestyle adjustments are the first line of defense. People who adopt a Mediterranean or plant-based diet lower their risk of cardiovascular disease by up to 30%, according to studies by the American Heart Association. Adding at least 150 minutes of moderate exercise weekly improves HDL levels and strengthens the endothelium (the inner lining of arteries), which prevents further damage. Even a 5–10% reduction in body weight can significantly lower triglycerides and improve blood sugar control, both of which contribute to healthier arteries.
At the same time, medical research is advancing. High-intensity statins and newer cholesterol-lowering drugs like PCSK9 inhibitors have been shown to shrink plaque and stabilize vulnerable deposits. Inflammation-targeting therapies, such as those tested in the CANTOS trial, demonstrate that reducing arterial inflammation can cut cardiovascular events even when cholesterol levels are already controlled. Emerging treatments focusing on ApoB, oxidized LDL (OxLDL), and lipoprotein(a) [Lp(a)] may further improve the possibility of reversing atherosclerosis in the near future. Scientists are also investigating ways to reverse arterial calcification, restoring flexibility to hardened arteries.
In summary, while atherosclerosis cannot be completely erased once advanced, a combination of lifestyle modifications and medical therapies can stabilize plaques, shrink early deposits, and drastically reduce the risk of cardiovascular complications.
Prevention Tips to Maintain Healthy Levels
Heart-Healthy Diet
- Eating more fruits, vegetables, whole grains, nuts, and omega-3 rich fish while avoiding processed foods and sugary drinks helps lower LDL and raise HDL.

Limit Unhealthy Fats
- Cutting down on saturated fats from red meat and dairy, and completely avoiding trans fats in fried and packaged foods, reduces plaque buildup in arteries.
Regular Exercise
- At least 150 minutes of moderate activity per week, such as brisk walking, cycling, or swimming, improves circulation, boosts HDL, and lowers LDL.
Maintain Healthy Weight
- Losing even 5–10% of excess body weight helps decrease LDL and triglycerides while improving insulin sensitivity and reducing risk of atherosclerosis.
Quit Smoking
- Stopping smoking restores healthy endothelium function, raises HDL levels, and cuts heart disease risk in half within a year.
Moderate Alcohol Use
- Limiting alcohol to one drink per day for women and two for men prevents high triglycerides, liver strain, and hypertension.
Manage Stress
- Practicing stress-relieving activities like meditation, yoga, or deep breathing lowers cortisol levels that indirectly worsen the level.
Regular Screenings
- Getting cholesterol levels checked every 4–6 years (or more frequently with risk factors) ensures early detection and better long-term prevention.
Living with High Cholesterol: Diet, Exercise, and Daily Care
High cholesterol management is a lifelong journey that requires consistency, discipline, and a commitment to daily healthy habits. It is not something that can be fixed once and forgotten; instead, it requires long-term planning and regular care.
Regular Cholesterol Monitoring is Essential
- Doctors recommend getting a lipid panel every 4–6 months if you have high cholesterol or are on medication.
- These tests measure LDL (bad cholesterol), HDL (good cholesterol), triglycerides, and in some cases advanced markers like ApoB or Lp(a).
- According to the CDC, 86 million U.S. adults have high cholesterol, but less than half manage it properly, showing how important routine testing is.
Medication Adherence Plays a Crucial Role
- Common drugs include statins, ezetimibe, and PCSK9 inhibitors, which lower cholesterol levels and reduce cardiovascular risks.
- Research from the American Heart Association shows that statins lower LDL by 30–50% when taken consistently.
- Missing doses, stopping suddenly, or self-adjusting medications can lead to arterial plaque buildup, increased risk of stroke, and coronary artery disease (CAD).
Dietary Changes Form the Foundation of Long-Term Management
- A heart-healthy diet rich in fruits, vegetables, whole grains, nuts, and lean protein helps keep cholesterol under control.
- Reducing foods high in saturated fats, trans fats, and cholesterol (like fried food, fast food, and processed meats) lowers LDL.
- Increasing foods with omega-3 fatty acids such as salmon, flaxseeds, and walnuts supports HDL (good cholesterol).
- Studies show that reducing saturated fat intake to less than 7% of total calories can cut LDL cholesterol by nearly 8–10%.
Exercise is Another Long-Term Strategy
- Engaging in at least 150 minutes of moderate-intensity activity per week (like brisk walking, swimming, or cycling) helps raise HDL and lower LDL.
- Strength training twice a week can improve metabolism and reduce body fat, which directly impacts cholesterol balance.
- Regular exercise also improves blood pressure, blood sugar control, and body weight, reducing overall cardiovascular risk.
Lifestyle Habits are Equally Important
- Quitting smoking helps HDL cholesterol rebound and protects the arteries from further damage.
- Limiting alcohol intake reduces triglyceride levels and prevents weight gain.
- Managing stress through meditation, yoga, or deep breathing lowers inflammation and indirectly improves lipid balance.
Consistency is the Key to Success
- People who combine diet, exercise, and medication adherence are far more successful at keeping cholesterol levels under control.
- Long-term success requires viewing cholesterol management not as a short-term treatment, but as an ongoing lifestyle commitment to protect the heart and arteries.
Conclusion
High cholesterol and arterial plaque buildup remain some of the leading risk factors for heart disease worldwide, but they are not unavoidable. While genetics and medical conditions can predispose someone to high cholesterol, lifestyle factors such as poor diet, lack of exercise, obesity, and smoking often accelerate the damage. The good news is that with the right approach, a heart-healthy diet, regular physical activity, weight management, medication when necessary, and consistent monitoring, cholesterol can be controlled, and plaque progression can be slowed or even reduced.
Research continues to highlight new therapies and medical interventions that give hope for reversing atherosclerosis, but prevention through healthy daily habits remains the strongest defense. By making mindful choices today, individuals can significantly reduce their risk of heart attack, stroke, and other cardiovascular complications, ensuring a longer, healthier life.
FAQs
Does high cholesterol cause plaque buildup in arteries?
Yes, high cholesterol, especially elevated LDL contributes to plaque buildup in arteries, leading to atherosclerosis and narrowed blood flow.
How long does it take for plaque to build up in arteries with high cholesterol?
Plaque buildup develops slowly over years or even decades, often starting in childhood but becoming noticeable in middle age.
What is the main cause of plaque buildup?
The main cause is excess LDL cholesterol combining with inflammation and damage in artery walls, forming fatty deposits.
What is the main source of cholesterol buildup and blockage in the arteries?
Unhealthy diet, smoking, lack of exercise, and genetic factors increase LDL cholesterol, which is the primary source of artery blockage.

 Medically reviewed by
Medically reviewed by