It is annoying to live with a sore stomach all the time. Chronic inactive gastritis occurs when the inflammation of the stomach lining is chronic with no exacerbations. This is a silent damage that can never be noticed until symptoms such as bloating or abdominal pains are experienced. This condition needs to be understood since it can cause gastric mucosal atrophy and other severe complications when it has not been treated. This article will explain about its causes, symptoms, histopathology and the way in which it should be treated to restore a healthy gut and have a better life every day.
WHAT IS CHRONIC INACTIVE GASTRITIS?
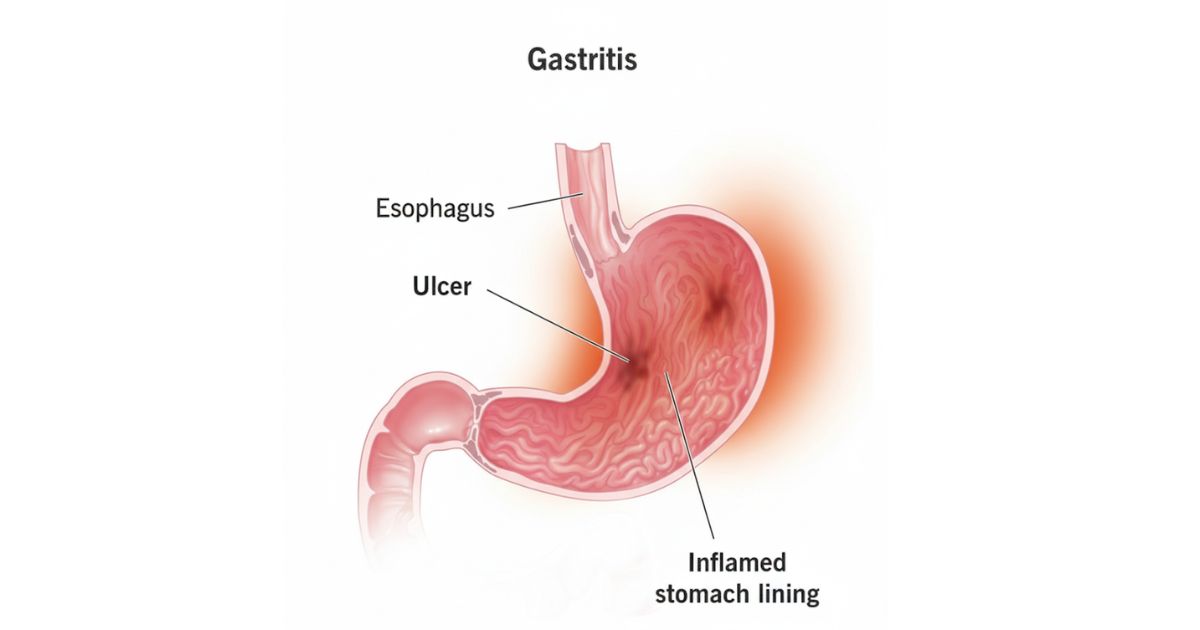
Chronic inactive gastritis is a problem in which the inflammation in the stomach lining is chronic but lacks the symptoms of active neutrophil inflammation. It implies that no acute attack occurs, but the mucosa of the stomach is destroyed. Physicians observe this in cases where a gastrointestinal tissue biopsy shows alterations in the form of plasma cell infiltration and destruction of the lamina propria. As opposed to acute gastritis, the pain may be acute; this is a silent condition and can take years before it manifests itself with symptoms.
CHRONIC INACTIVE VS. CHRONIC ACTIVE GASTRITIS: MAJOR DIFFERENCES
The primary distinction is in the microscopic image observed in the histopathology. Pathologists observe the presence of neutrophils in chronic active gastritis, which is an indication of active irritation. In active gastritis that is chronic and inactive, neutrophils are absent but still depict signs of chronic inflammation. Here is a quick comparison:
| Feature | Chronic Active Gastritis | Chronic Inactive Gastritis |
| Neutrophils | Present | Absent |
| Pain Flare-ups | Common | Mild/Silent |
| Mucosal Damage | Persistent | Partially healed |
| Progression Risk | Greater | Less but Still Greater |
This difference is important since the mode of treatment varies as to whether the stomach is still in the process of attack.
IN THE U.S. PREVALENCE AND EPIDEMIOLOGY
In the United States, studies indicate that chronic gastritis is present in close to 30 percent of adults who are above 50 years old and much of these cases are chronic non-infectious gastritis. This prevalence is high indicating that several people are living their lives with silent injury to their gastric mucosa. The disease is not recognized most of the time until its symptoms turn to be irritating or the gastric biopsy under routine check-ups depicts persistent alterations. This is where the significance of early identification is given, especially in individuals who have a predisposition to such risk factors as NSAIDs overuse or excessive alcohol intake.
The National Institutes of Health claim that approximately one-third of Americans (35 percent) have Helicobacter pylori infection and it is one of the most common causes of gastritis. This bacteria may remain in years causing silent destruction of the protective mucus layer, which results in plasma cell invasion. With time, the untreated cases can progress into the gastric mucosal atrophy or even intestinal metaplasia, which increases the chances of severe complications. The early stage of testing and treatment are necessary measures to ensure the protection of stomach health in the long term and avoid further harm.
THE SIGNS AND SYMPTOMS AND EARLY WARNING OF CHRONIC INACTIVE GASTRITIS
This disease is a silent one and in most cases, builds up over time. Individuals can experience pains that are intermittent and others may not experience at all until the situation escalates. Early identification of these signs can help a lot in the prevention of complications.
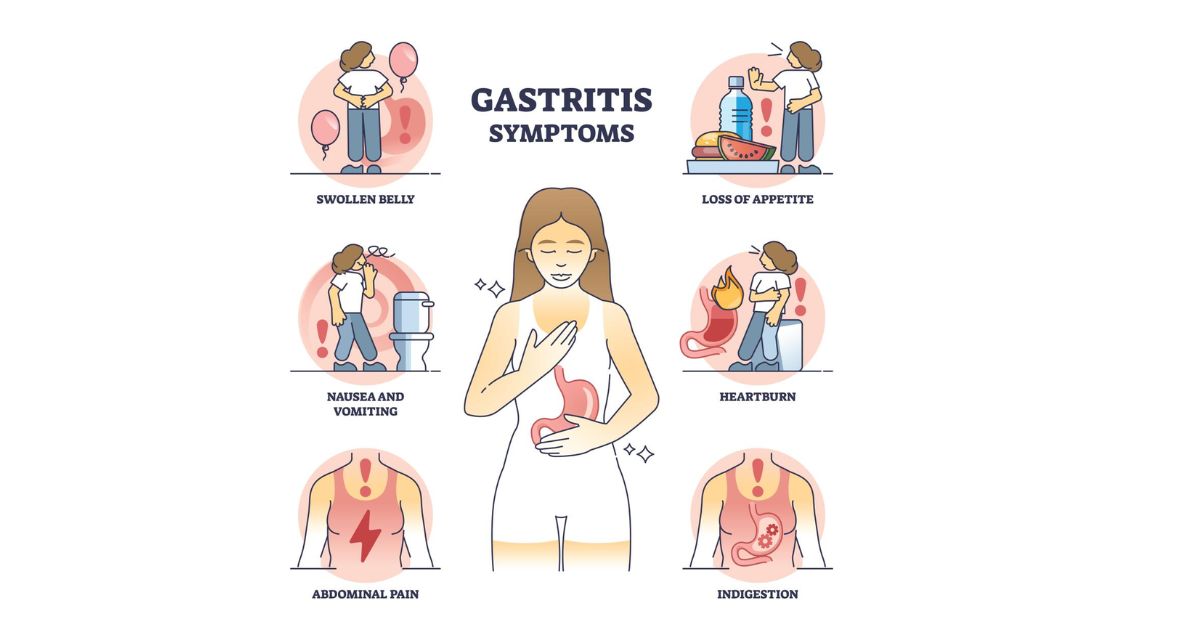
- Abdominal pain
- Epigastric burning
- Bloating
- Nausea
- Vomiting
- Loss of appetite
- Weight loss
Due to the subtlety and mildness of the symptoms, there are those who take time to visit a doctor. The damage to the gastric mucosa can be detected before it intensifies in case of early screening and a timely gastric biopsy.
COMMON CAUSES AND HAZARDOUS FACTORS
The causes of chronic inactive gastritis are heterogeneous and most of them tend to accumulate with time. The individual causes have a specific effect in harming the gastric mucosa and predisposing to chronic inflammation.
NSAID Overuse
NSAID-induced gastritis may be produced by the long usage of pain relievers such as ibuprofen or aspirin. These drugs lower the protective mucus lining in the stomach and hence expose the stomach lining to harm. This will cause micro-tears and persistent irritation with time which ultimately causes inactive changes that are chronic.
Alcohol Consumption
Regular alcohol consumption is capable of damaging gastric epithelium, irritating the lamina propria and raising acid secretion. Such continuous exposure undermines the natural protection of the stomach, slows down the healing of tissue and provides conditions to permanent gastritis.
Autoimmune Conditions
The immune system of the body in the case of autoimmune gastritis wrongly attacks the foveolar cells and other components of the stomach lining. This immune reaction leads to the thinning of the gastric mucosa and may eventually result in gastric mucosal atrophy which causes nutrient malabsorption and additional complications.
Bile Reflux
Bile reflux gastritis occurs when bile discharged into the small intestine moves back to the stomach. This chemical damage erodes the lining and aggravates the process of plasmid cell infiltration leading to chronic inflammation and failure of the mucosal injury to be repaired over time.
HELICOBACTER PYLORI AND ITS ONSET IN CHRONIC INACTIVE GASTRITIS
H. pylori bacteria is one of the most prevalent agents that cause chronic inactive gastritis. It is a spiral microbe that interferes with the secretion of gastric acid and gradually worsens the gastric epithelium. The damage it does leads to the depletion of the protective mucus layer and exposes the stomach to chronic inflammation. The damage goes on in the background even with mild symptoms, so it goes unnoticed, hence the disease moves undetected.
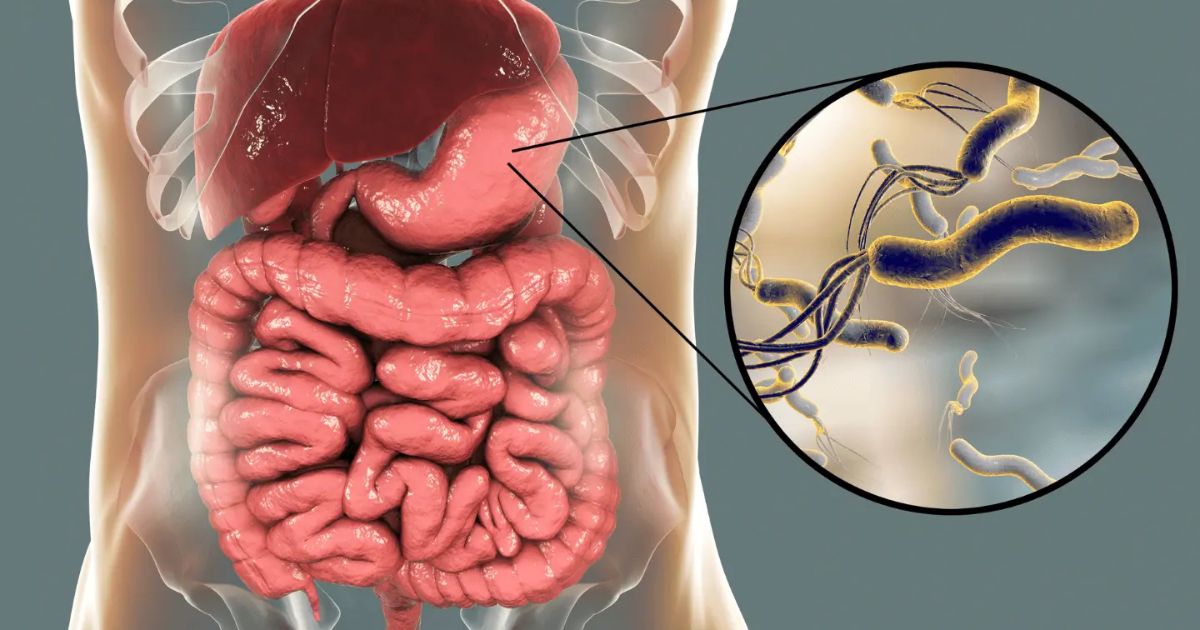
Unattended, Helicobacter pylori infection can result in the degradation of the mucosa of the stomach by the infiltration of plasma cells, gastric atrophy, and ultimately to intestinal metaplasia, which is a precancerous alteration. Early diagnosis and treatment of this infection with antibiotics in case of H. pylori and acid-reducing therapy helps to eliminate the shift between chronic active and chronic inactive gastritis and provide the stomach lining with an opportunity to regenerate properly.
DIAGNOSTIC TECHNIQUES: ENDOSCOPY, BIOPSY AND BLOOD TESTS
To identify the presence of chronic inactive gastritis, as well as its etiology, doctors use a number of accurate diagnostic procedures. Due to the fact that this condition tends to be mild or even silent, it is vital to detect it early to prevent gastric mucosal atrophy or intestinal metaplasia over a long period of time.
- Endoscopy
- Gastric biopsy
- Histopathology report
- Blood tests
- Stool antigen tests
- Immunohistochemistry
- Urea breath test
- Autoimmune markers serology
Endoscopy enables a direct observation of gastric lining whereas a gastric biopsy gives us tissue to study in detail under histopathology. These specimens display the presence of such characteristics as plasma cell infiltration, foveolar cell loss, and lamina propria structural damage. Blood tests, stool antigen tests and breath tests assist in reinforcing H. pylori infection and influence treatment decisions. Further methods such as immunohistochemistry provide even better classification of chronic inflammation and allow distinguishing autoimmune gastritis and NSAID-induced gastritis among other subtypes.
ROOT CAUSE AND CLASSIFICATION AT THE HISTOLOGICAL LEVEL
The Sydney System is commonly used by pathologists in categorizing the types of gastritis, even in the case of chronic inactive gastritis. This system facilitates the standardization of reporting with the help of analysis of such features as chronic inflammation, gastric mucosal atrophy and intestinal metaplasia. The most important factor in preventing damage to the gastric mucosa further and recovering the balance is to find the root cause.
Chronic Inflammation
This is characterized by the presence of plasma cell infiltration and destruction of the lamina propria. It means that the stomach lining was irritated in the course of time and became permanently inactive with the persistent inflammation.
Gastric Mucosal Atrophy
This is a phase that is characterized by the thinning of the stomach wall and the loss of functional glands. It has an ability to reduce secretion of gastro acid, influence digestion and make a person vulnerable to infections.
Intestinal Metaplasia
This stage is considered a precancerous change; it demonstrates the substitution of cells of gastric epithelium with cells of the intestine type. The fact that the structure of the stomach is being changed because of an old-time trauma is an alarming sign.
Root Causes
The key causes are the infection of Helicobacter pylori, excessive use of NSAIDs, autoimmune gastritis, and bile reflux gastritis. All of these interfere with the protective layer of the mucus and slow down the process of healing the tissue, which leads to the further development of the condition without treatment.
GOOD TREATMENT PRACTICES AND THERAPEUTIC INTERVENTIONS
Treatment of chronic inactive gastritis is not just the relief of pain or discomfort. I think that early treatment can be very important in avoiding the gastric mucosal atrophy and preventing the development of the more severe conditions such as intestinal metaplasia. The appropriate treatment is aimed at the etiological agent and the ensuing chronic inflammation, which will enable appropriate healing of the tissue and recovery of the gastric epithelium.

- H. pylori eradication Antibiotics
- Proton Pump Inhibitors (PPIs) to stop the secretion of gastrointestinal acid
- Drugs which enhance the protective lining of the mucus
- Stop of NSAIDs and replace with safer ones
- Toxicated autoimmune gastritis injections with vitamin B12
- Treatment of bile reflux gastritis using bile acid binders
The prompt and specific treatment can prevent the further damage, decrease the infiltration of plasma cells, and restore the normal functioning of the stomach. Also, completion of therapy reduces the risk of complications in the long run.
NUTRITIONAL ADAPTATIONS AND CHANGES IN LIFESTYLE TO HEAL
Healing takes commitment. Researchers suggest such lifestyle changes as alcohol cessation, stress management, and mindful eating. Dietary modification may involve consumption of smaller and repeated meals and the inclusion of foods that are highly probiotic to help normalize the stomach environment. Small meals were found to help many of the patients recover faster in my experience. It has been shown to reduce spicy and acidic foods which aid in accelerating the healing of the gastric epithelium.
RISKS OF NOT TREATED IN GOOD TIME
Failure to address this situation hastens to gastric mucosal atrophy, ulcers or even stomach cancer in extreme cases. Prolonged irritation is a risk that leads to intestinal metaplasia and subsequent dysplasia. The positive thing is that all these risks can be lowered considerably with early diagnosis by endoscopy and treatment.
PREVENTION AND MANAGEMENT LONG-TERM MANAGEMENT
Living with chronic inactive gastriocarcinoma requires one to be proactive. In my opinion, frequent examinations are essential in case you experience gastritis in the past. Regular follow-up appointments, regular gastric biopsy when necessary, and attentive attention to symptoms are some of the ways to maintain the situation at bay. Some of the preventive tools include a balanced diet, exercise, and alleviation of stress. Being vigilant to emerging symptoms will make sure that it is acted upon.
CONCLUSION
Inactive gastritis can be chronic and it may appear harmless as it is silent but it still refers to the damage of the gastric mucosa. The primary step to safeguard your stomach is to know what causes it, what its symptoms are and how you can treat it. You can go through small and regular adjustments and restore balance to improve your quality of life.
FAQs
1. What is chronic inactive gastritis and what is the method of its diagnosis?
Chronic inactive gastritis is a chronic inflammation of the stomach lining, which is not neutrophil-infiltrated. It is determined by endoscopy and gastric biopsy.
2. Is chronic inactive gastritis reversible into stomach cancer?
Yes, when untreated it may result into gastric mucosal atrophy and intestinal metaplasia, which may predispose to cancer in the long run.
3. What is the pathophysiology of H. pylori infection to chronic inactive gastritis?
The bacteria H. pylori destroy the protective mucus covering and interfere with gastric acid secretion, which results in the chronic inflammation which can be inactive.
4. Which is the most appropriate mode of treatment of chronic inactive gastritis?
Antibiotics against H. pylori, proton pump inhibitors, a change in lifestyle, and a change of diet are used to treat.
5. Will diet and lifestyle change manage chronic inactive gastritis?
Yes: preventing the overuse of NSAID, limiting the intake of alcohol, eating small portions, and using probiotics can be used to prevent and control episodes.

 Medically reviewed by
Medically reviewed by