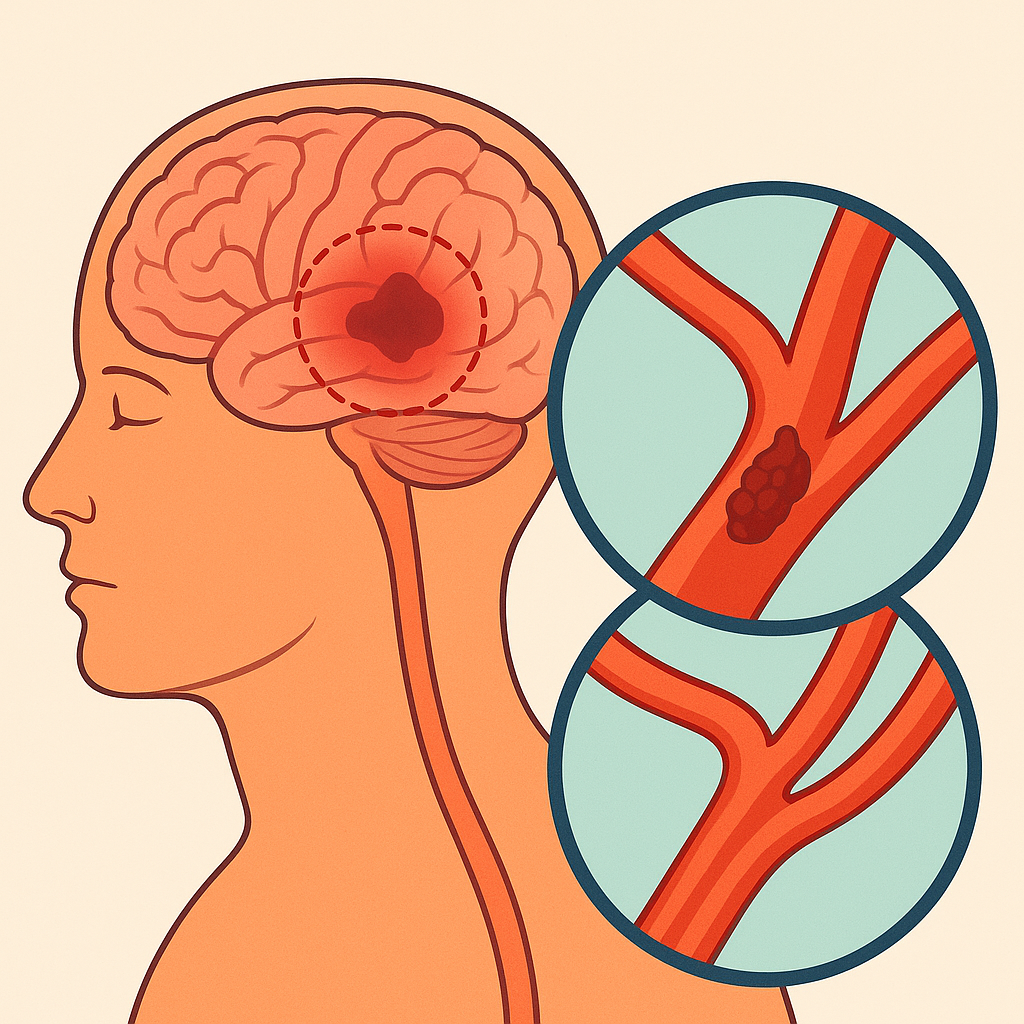
When I first learned about cryptogenic stroke, I was struck by how something so serious could remain without a known cause, even with today’s advanced diagnostic tools. A stroke occurs when blood flow to the brain is interrupted by a clot or blockage, leading to ischemia or even infarction. What makes cryptogenic strokes particularly challenging is that, despite extensive diagnostic tests and imaging, the definitive cause often remains unknown. This condition is life-threatening and demands immediate medical attention and emergency care.
From my experience working alongside neurologists, cardiologists, and electrophysiologists, I have seen how team-based investigation is key to identifying potential causes. Each specialist explores factors such as atrial fibrillation (AFib), structural heart defects, or clotting disorders like thrombophilia. Advanced diagnostic tools, including intracranial imaging, cardiac monitoring, and transesophageal echocardiography, help search for hidden mechanisms. Still, even with modern technology, some patients are left without clear answers a reminder of how complex this condition truly is.
Causes and Risk Factors
Heart Related Triggers
Many experts have observed that cryptogenic stroke often links back to hidden heart conditions. Across the U.S., about 5.2 million people live with atrial fibrillation (AFib) an irregular, sometimes rapid heart rhythm. In AFib, the upper chambers (atria) beat inefficiently, reducing effective blood flow throughout the body. This disruption allows clots to form in the left atrium, which may then travel to the brain and trigger a stroke.
Common AFib symptoms include palpitations, fatigue, and shortness of breath, though the condition can also remain asymptomatic. Because AFib episodes can be infrequent, continuous heart rhythm monitoring is crucial. Physicians often prescribe anticoagulants or anti-clotting medications to lower stroke risk, as AFib increases the likelihood of stroke by more than five times.
Another important heart-related cause is Patent Foramen Ovale (PFO) a small opening between the right and left atria that normally closes after birth. In some adults, incomplete closure allows blood to bypass the lungs, potentially carrying clots directly to the brain. Depending on severity, surgical closure of the PFO may be recommended to prevent recurrence.
Blood and Vascular Conditions
Certain blood disorders and vascular abnormalities can also contribute to cryptogenic stroke. Hypercoagulable states or thrombophilic conditions increase the blood’s tendency to clot. These may be inherited or acquired and are often identified through specialized testing. Studies show that 1 in 7 patients with cryptogenic stroke test positive for thrombophilia. Though uncommon, rapid clot formation can block cerebral vessels and cause severe outcomes.
Another vascular factor is Aortic Arch Atheroma the buildup of fatty plaques within the aorta, the body’s largest artery. This atherosclerosis hardens and narrows arteries, reducing blood flow and heightening the risk of embolic events. Contributing factors include high blood pressure, diabetes, smoking, and elevated LDL cholesterol, all of which increase the risk of both heart disease and stroke.
Other Rare Causes and Awareness
Some cryptogenic strokes are linked to less common conditions, including cancer-related hypercoagulability, infections such as endocarditis (inflammation of the heart’s inner lining), or arterial dissection a tear in the artery wall. Though rare, these causes can be life-threatening if not recognized early.
Symptoms and Early Warning Signs
Common Neurological Symptoms
Cryptogenic stroke shows sudden onset of neurological symptoms similar to other ischemic strokes. Key warning signs follow the FAST rule Face drooping, Arm weakness, and Speech difficulty.
Other common symptoms include:
- Loss of sensation or reduced strength on one side of the body
- Sudden vision loss or double vision
- Loss of balance or coordination
- Severe headache with no known cause
- Confusion or difficulty understanding speech
Cortical symptoms such as aphasia, hemianopia, and gaze deviation may appear in embolic or cryptogenic cases.
Atypical or Subtle Presentations
Not all patients show classic stroke signs some have non-traditional or mild symptoms. Younger patients may have rare or unusual causes like arterial dissection or thrombophilia.
Posterior circulation strokes may cause:
- Vertigo, dizziness, or imbalance
- Double vision or blurred vision
- Nausea or vomiting
Subtle warning signs may include:
- Temporary numbness, confusion, or visual changes
- Short-term behavioral or cognitive changes
Transient Ischemic Attacks (Mini-Strokes)
A Transient Ischemic Attack (TIA) is a brief episode of neurological dysfunction without permanent brain damage. Symptoms usually resolve within minutes to hours, but it serves as a serious warning sign of stroke.
Rapid evaluation after a TIA helps detect hidden embolic sources or heart rhythm abnormalities like AFib.
Studies show:
- 3–10% risk of stroke within 2 days after TIA
- 5–17% risk within 90 days
Diagnosis and Medical Evaluation
Understanding how doctors identify cryptogenic stroke is essential because the cause is often hidden despite advanced technology. The diagnostic process involves several steps to rule out known causes of stroke and detect underlying heart or vascular problems.
Initial Clinical Assessment
- The process usually begins with a neurological exam and a detailed medical history.
- Doctors check for symptoms such as weakness, speech difficulty, or vision changes.
- Immediate tests like blood pressure monitoring, blood sugar, and cholesterol levels help identify common risk factors.
Brain and Vascular Imaging
- A non-contrast CT scan is often the first test to confirm a stroke and exclude bleeding.
- MRI with diffusion-weighted imaging (DWI) is more sensitive and helps detect small or early brain lesions.
- CT or MR angiography and carotid ultrasound visualize the arteries supplying the brain, revealing any blockage or narrowing.
Cardiac Evaluation
- Since many cryptogenic strokes may stem from hidden heart issues, cardiac testing plays a key role.
- Echocardiography checks for heart defects such as Patent Foramen Ovale (PFO) or clots.
- A 12-lead ECG records the heart’s rhythm, while extended cardiac monitoring (like a loop recorder) detects silent atrial fibrillation, a major hidden cause.
- Studies show that long-term monitoring can identify undetected AFib in nearly 30% of patients initially classified as cryptogenic.
Laboratory and Specialized Tests
- Blood tests may reveal clotting disorders, inflammation, or infections.
- Doctors often evaluate for thrombophilia, autoimmune diseases, or metabolic syndromes that can increase stroke risk.
- When standard tests fail to show the cause, advanced cardiac imaging or implantable monitors may be used for continuous observation.
Treatment and Management
Immediate Stroke Care
When a patient arrives with symptoms of stroke, immediate treatment is critical. Doctors often follow the same emergency protocol used for ischemic strokes.
- Intravenous thrombolysis (IV tPA) may be given within the first 4.5 hours to dissolve a clot if the patient qualifies.
- In some cases, mechanical thrombectomy a minimally invasive procedure to remove a clot can be performed up to 24 hours after symptom onset.
- Every minute counts, as prolonged blockage can lead to irreversible brain damage.
In my experience observing stroke care units, teamwork makes a clear difference rapid imaging, swift decision-making, and synchronized communication among specialists often determine survival and recovery outcomes.
Medications and Antithrombotic Therapy
Once the emergency phase is controlled, attention shifts to secondary prevention.
- For most patients without a confirmed cause, antiplatelet therapy (such as aspirin or clopidogrel) is the preferred treatment.
- Studies like NAVIGATE ESUS and RE-SPECT ESUS found no clear benefit of using direct oral anticoagulants (DOACs) over aspirin in preventing recurrent cryptogenic strokes.
- If tests later reveal a Patent Foramen Ovale (PFO) or other high-risk heart condition, doctors may recommend anticoagulation therapy or PFO closure surgery to stop future clots from reaching the brain.
Rehabilitation and Recovery Strategies
Recovery doesn’t end after hospital discharge it’s a long journey requiring dedication and structured care.
- Physical and occupational therapy help regain lost motor function and coordination.
- Speech and cognitive therapy are vital for patients who experience communication or memory issues.
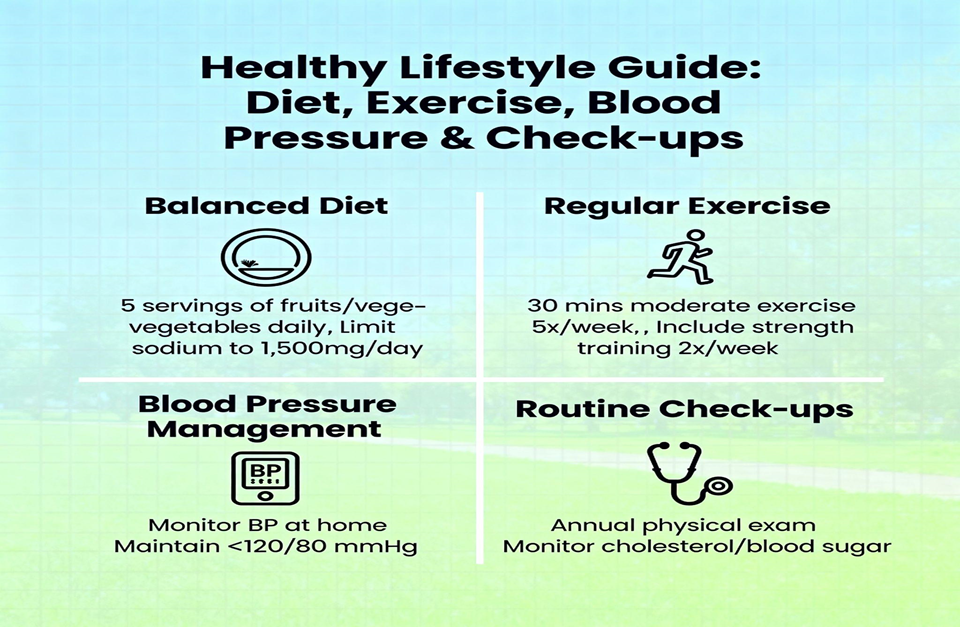
- Beyond therapy, lifestyle changes play an equally strong role: controlling blood pressure, quitting smoking, managing diabetes, and maintaining healthy cholesterol levels significantly reduce recurrence risk.
- The American Heart Association’s Life’s Essential 8 emphasizes habits like balanced nutrition, exercise, and medication compliance to reduce recurrence.
From what I have seen, consistent encouragement and family involvement greatly enhance motivation during rehabilitation. Progress may be slow, but steady efforts lead to meaningful recovery.
Long-Term Follow-Up and Monitoring
Because cryptogenic stroke often hides an underlying cardiac or vascular cause, long-term monitoring becomes essential.
- Patients may undergo extended rhythm monitoring through wearable devices or implantable loop recorders to detect hidden atrial fibrillation (AFib) found in up to 30% of cases over time.
- Regular follow-ups with both neurology and cardiology teams ensure that any late-appearing abnormalities are caught early.
- For younger patients with PFO, closure combined with antiplatelet therapy has shown improved long-term outcomes.
Real-Life Perspective: A Stroke Survivor’s Story
A 38-year-old female patient, otherwise healthy and with no prior history of hypertension, diabetes, or heart disease, presented to the emergency department with sudden-onset weakness of the right upper limb and mild slurring of speech. Initially, the symptoms were dismissed as fatigue or stress-related. However, neurological assessment and imaging confirmed an ischemic event consistent with a cryptogenic stroke.
Further diagnostic evaluations, including cardiac monitoring, vascular imaging, and coagulation studies, revealed no definitive cause, fitting the criteria for a cryptogenic etiology. The patient was initiated on antiplatelet therapy and later enrolled in a comprehensive stroke rehabilitation program focusing on motor function and speech recovery.
Over several months, the patient demonstrated significant neurological improvement and regained functional independence. Her case highlights the importance of early recognition, timely intervention, and ongoing follow-up in suspected stroke cases even in individuals without traditional risk factors. It also emphasizes the continuing need for research into underlying mechanisms and preventive strategies for cryptogenic stroke in younger populations.
Research and Future Directions
Long-term rhythm monitoring devices and wearable ECG technology are revealing hidden arrhythmias that traditional short-term tests often miss. Scientists are exploring genetic markers, advanced imaging techniques, and blood biomarkers to pinpoint subtypes of cryptogenic stroke more precisely. Ongoing trials are refining when and for whom PFO closure or anticoagulants may truly work best.
The search for answers continues globally. Researchers are uncovering new insights into genetic, environmental, and vascular factors linked to cryptogenic strokes. Studies show African-Americans and Hispanics are twice as likely to experience this type of stroke. Collaborative, ongoing research supported by communication between healthcare teams, patients, and families plays a vital role in uncovering the hidden mechanisms behind this unexplained medical condition.
Conclusion
Cryptogenic stroke stands as one of the most perplexing challenges in modern neurology a condition defined not by what we know, but by what remains hidden. Despite extensive diagnostic tools and multidisciplinary collaboration, many cases still defy explanation. Yet, progress is undeniable. From cutting-edge cardiac monitoring to genetic research and lifestyle-centered prevention, every stride brings us closer to decoding this medical mystery.
Through the lens of both clinical experience and patient stories, one thing becomes clear: early detection, comprehensive care, and persistent follow-up save lives. For patients, understanding their condition and staying actively involved in prevention is just as critical as medical treatment itself. For professionals, cryptogenic stroke serves as a reminder that medicine is as much about discovery as it is about healing demanding empathy, vigilance, and innovation at every step.
FAQ’s
1. What is the difference between ischemic and cryptogenic stroke?
An ischemic stroke occurs when a known cause usually a blood clot or blocked artery restricts blood flow to the brain.
A cryptogenic stroke, on the other hand, is a type of ischemic stroke where no definitive cause can be identified even after extensive testing. It accounts for roughly 25–40% of all ischemic strokes, making it one of the most puzzling stroke categories.
2. What are the four types of strokes?
The four main types include:
- Ischemic stroke – caused by a clot blocking blood flow to the brain.
- Hemorrhagic stroke – due to bleeding from a ruptured vessel.
- Transient Ischemic Attack (TIA) – often called a “mini-stroke,” a temporary blockage without lasting damage.
- Cryptogenic stroke – an ischemic stroke with no clearly determined cause.
3. What does cryptogenic mean in medical terms?
In medical terminology, “cryptogenic” means “of unknown origin.” When used with “stroke,” it describes a brain ischemic event where the underlying source of the blockage remains unidentified despite comprehensive cardiac, vascular, and hematologic evaluations.
4. Is a TIA the same as a cryptogenic stroke?
No, A Transient Ischemic Attack (TIA) is a temporary disruption of blood flow to the brain that doesn’t cause permanent tissue damage.
A cryptogenic stroke, however, involves lasting neurological injury, even though its exact cause remains uncertain.
Both conditions share overlapping symptoms, and a TIA can sometimes be a warning sign before a future cryptogenic or ischemic stroke

 Medically reviewed by
Medically reviewed by