Erythematous Candidiasis, also called atrophic oral candidiasis, is a common form of oral fungal infection by Candida albicans. This disorder causes the oral mucosa to become reddened, painful, and inflamed. Although it can still be mild at the beginning, when untreated, it can be very uncomfortable and can signify other long-term health problems, such as a poorly functioning immune system or extensive antibiotic consumption. To prevent and treat erythematous candidiasis, it is essential to understand its causes and risk factors as well as to know how it is managed.
What is Erythematous Candidiasis?
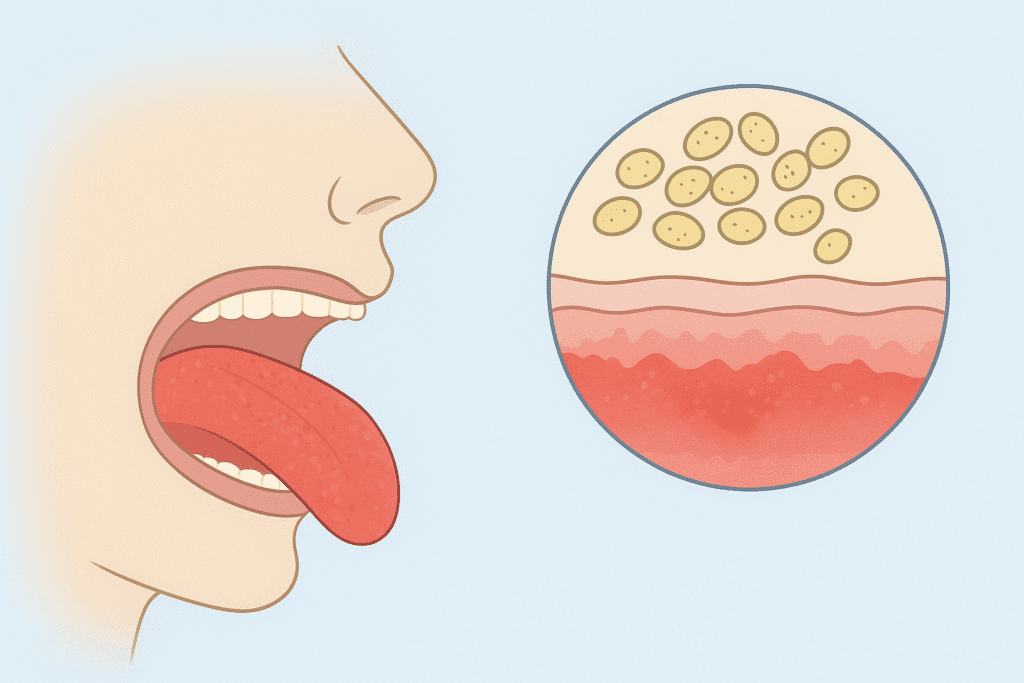
Erythematous candidiasis is a subtype of oral candidiasis that appears as red, inflamed patches on the tongue, palate, or other parts of the mouth. Unlike pseudomembranous candidiasis (commonly known as oral thrush), this type does not present with white plaques. Instead, the affected areas appear smooth, shiny, and erythematous (red). This condition often develops after the use of broad-spectrum antibiotics, steroid inhalers, or due to dentures, which disrupt the natural balance of microorganisms in the oral cavity.
Aetiology and Pathogenesis
Candida albicans is the predominant causative organism, a yeast-like fungus that is normally harmless in the mouth. This fungus can also develop into a pathogenic form under some conditions and cause infection. Immunosuppression, xerostomia (dry mouth), diabetes mellitus, and prolonged use of antibiotics can facilitate this transition.
Candida glabrata and Candida tropicalis, other non-albicans species of Candida, can also cause erythematous candidiasis, particularly in immunocompromised patients. The fungus sticks to the epithelial cells of the mucosa of the mouth, releasing enzymes and toxins that affect the tissue and cause inflammation.
Types of Candidiasis Erythematous
Erythematous Candidiasis has two clinical manifestations:
1. Acute Erythematous Candidiasis
This type of development is sudden and can be associated with antibiotic treatment. Patients complain of a burning sensation on the tongue and of redness, particularly on the dorsal side. Destruction of the filiform papillae leaves the tongue shiny. The condition is normally resolved by stopping antibiotics and starting antifungal treatment.
2. Chronic Erythematous Candidiasis
This category is more chronic and often is linked to the wearers of dentures, particularly denture wearers who wear them 24 hours a day, even at night. The disease mostly attacks the denture area of the palate, causing denture stomatitis. It can also be present in immunocompromised people, including those with HIV/AIDS or uncontrolled diabetes, in certain cases.
Risk Factors
There are a number of risk factors that lead to erythematous candidiasis, and most of these risk factors disrupt the balance of microorganisms inherent to the mouth porta.
The main risk factors include:
- Prolonged use of antibiotics: Particularly the broad-spectrum antibiotics which inhibit normal bacterial flora and result in overgrowth of Candida species. These are one of the most common factors.
- Use of inhaled steroids: Patients taking inhaled steroids to treat asthma or chronic obstructive pulmonary disease (COPD) have a higher risk of infection, especially when they fail to rinse their mouths following inhalation.
- Diabetes mellitus: A high concentration of glucose poses the perfect condition in which fungi thrive and impedes immune defence systems.
- Weakened immunity: Individuals with weakened immunity, like those with HIV/AIDS, or those receiving chemotherapy or organ transplants, do not have an intact immune system to control Candida.
- Use of dentures: The use of dentures is another significant predisposing condition, particularly when dentures are ill-fitting or unclean or worn continuously, including at the time of sleep.
- Smoking: Smoking is another risk factor that changes oral pH, reduces oxygen concentration, and damages mucosal tissues, promoting fungal growth.
Clinical Features of Erythematous Candidiasis
General Appearance
Redness and tenderness of the oral mucosa, especially on the reverse side of the tongue, palate, or buccal mucosa, is the main clinical manifestations of erythematous candidiasis.
Characteristics
The erythematous candidiasis is smooth, shiny, red, and may be painful or cause a burning sensation, usually in contrast to the pseudomembranous candidiasis, which is white and removable (plaques).
Symptoms
Patients usually complain of pain during the consumption of hot, salty or acidic foods. Loss of taste (dysgeusia) or an unattractive metallic taste of the mouth may be present in some cases. The tongue is frequently depapillated and is glossy or bald, the filiform papillae having been lost.
In Denture Wearers
However, in patients with dentures, erythematous candidiasis is most common in the form of denture stomatitis, where the redness is limited to the location under the denture base, especially in the palate. The disorder can be asymptomatic or can lead to mild soreness and swelling.
Severe or Chronic Cases
In less minor or chronic situations, there may be pain upon swallowing, or odynophagia, particularly when the infection spreads into the throat. Although these symptoms are not life-threatening, they may be extremely uncomfortable and impact eating patterns and oral health in general.
Diagnosis
A diagnosis of erythematous candidiasis is made by a combination of laboratory tests and clinical examination. At the oral exam, the clinician will notice the typical red shiny mucosal areas and evaluate the medical and dental history of the patient to determine potential risk factors, such as antibiotic or steroid use. Lab confirmation can aid in distinguishing candidiasis and other mouth lesions. A smear, or swab test, is often done, whereby the swab or sample taken is studied under a microscope with a potassium hydroxide (KOH) preparation, which shows the presence of fungus hyphae and budding yeast cells. Detection of the exact Candida species is achieved by culture tests on Sabouraud dextrose agar.
When initial treatment fails or the condition recurs, molecular diagnostic tests should be applied using polymerase chain reaction (PCR) to determine resistant strains of Candida. In some cases, a biopsy is necessary to rule out other mucosal diseases such as precancerous lesions or chronic atrophic glossitis.
Erythematous Candidiasis Treatment
Treatment of erythromycin-resistant candidiasis aims at curing the fungus, reestablishing the oral microflora, and treating underlying factors.
Topical Antifungal Therapy
Topical antifungal agents are typically used as a starting point in treatment and are very effective in mild to moderate cases. Such drugs as Nystatin oral suspension, Clotrimazole troches, and Miconazole gel, which inhibit the synthesis of the fungal cell wall, are commonly used.

These are used in multiple doses a day, typically for between one and two weeks, until symptoms disappear.
Systemic Antifungal Therapy
Systemic antifungal therapy might be required in more serious or persistent infections, with preference given to Fluconazole (100–200 mg/day) or Itraconazole (100 mg/day) because of their good oral bioavailability and efficacy against resistant strains.
Correction of Predisposing Factors
Closely related to the correction of predisposing factors is important. Patients are encouraged to stop taking unnecessary antibiotics, control blood sugar levels (when diabetic), and take better care of their dentures by removing them at night and cleaning them daily.
People who take inhaled corticosteroids are advised to rinse their mouths with every use to avoid the accumulation of fungi.
Oral Hygiene and Supportive Care
Good oral hygiene with frequent brushing, flossing, and application of antiseptic mouthwash like chlorhexidine gluconate plays a significant role in reducing Candida colonisation. Saliva substitutes or sugar-free chewing gum can be used to replace saliva lost in dry mouth.
Prevention and Self-Care
Erythematous candidiasis prevention is mainly focused on a healthy mouth and control of risk factors.
Oral Hygiene Practices
Good oral health and dental brushing twice a day, tongue cleaning, and denture disinfection can minimise the number of fungi. It is important that a denture wearer should take out the dentures at night and leave them in an antifungal and disinfectant solution.
Blood Sugar Control
Individuals with diabetes need to regulate the level of sugar in their blood since unregulated glucose largely encourages the development of Candida.
Inhaled Corticosteroid Users
Individuals taking inhaled corticosteroids should always rinse their mouth after taking inhalers to reduce fungal growth.
Lifestyle Habits
Oral health is also promoted by avoiding smoking and excessive alcohol consumption since both affect the mucosal defences by changing oral pH.
Nutrition and Hydration
Maintaining hydration and eating a healthy diet with plenty of vitamins and minerals will help in the working of the immune system work and repair the oral tissue.
Dental Check-ups
Dental check-ups should be conducted regularly to detect any mucosal or fungal changes.
Erythematous Candidiasis in Immunocompromised Patients
The erythematous candidiasis is more severe, persistent, and recurrent in the immunocompromised individuals,; HIV/AIDS, cancer, organ transplantation patients, etc. Their compromised immunity gives the Candida species a chance to enter deeper tissues and develop resistance against conventional antifungal treatment. These patients may need prophylaxis with antifungal agents as well as close observation under the care of medical professionals.
Oral checkups are very important to detect early infection before it can reach the oesophagus or the pharynx. Treatment of the underlying immunosuppression condition in association with antifungal therapy offers improved outcomes and minimises recurrence risk. These patients need nutritional support, dietary measures, and careful oral hygiene to have a stable oral ecosystem.
Conclusion
Erythematous candidiasis is another frequently occurring but underdiagnosed oral fungus and needs to be identified and treated as soon as possible. Knowing how it relates to other factors, such as antibiotic use, immunosuppression, and poor oral hygiene, is useful in prevention and treatment. Antifungal treatment, oral healthcare, and lifestyle changes can help patients recover fully and avoid relapse. Dentist visits and/or knowledge of the initial symptoms will provide early treatment and ensure that you have a healthy and infection-free mouth.
FAQ’s
What are the causes of erythematous candidiasis?
It is primarily due to Candida albicans overgrowth because of factors such as antibiotics, dentures, diabetes, or poor immunity.
2. What is the difference between oral thrush and it?
Oral thrush (pseudomembranous candidiasis) appears white, whereas erythematous candidiasis appears red, smooth, and devoid of white coating.
3. Am I able to treat erythematous candidiasis at home?
Light cases respond to good oral care and antifungal mouthwash; however, the chronic cases require medical attention.
4. Is candidiasis erythematous contagious?
It is not very contagious, although in some cases it can be transmitted through direct contact, particularly when oral hygiene is poor.
5. How long does it take to heal?
Most cases can be cured in 7-14 days, although chronic ones can be more difficult.
6. Can it come back?
Yes, it may recur when other risk factors like denture use or diabetes are not properly handled.

 Medically reviewed by
Medically reviewed by