Preeclampsia is a condition that is present in millions of pregnant women across the world and is one of the most difficult hypertensive disorders of pregnancy. The question among numerous individuals is: does it have a genetic or lifestyle predisposition? It has been found out that genetic predisposition and environment triggering are determinants of a woman at risk. Researchers have discovered the candidate genes and studied the role of regulation of gene expression in the placenta, blood flow, and general health of the pregnancy. Knowledge of this balance of nature and nurture would allow families to be better prepared and achieve better outcomes in mothers and babies.
What is Preeclampsia?
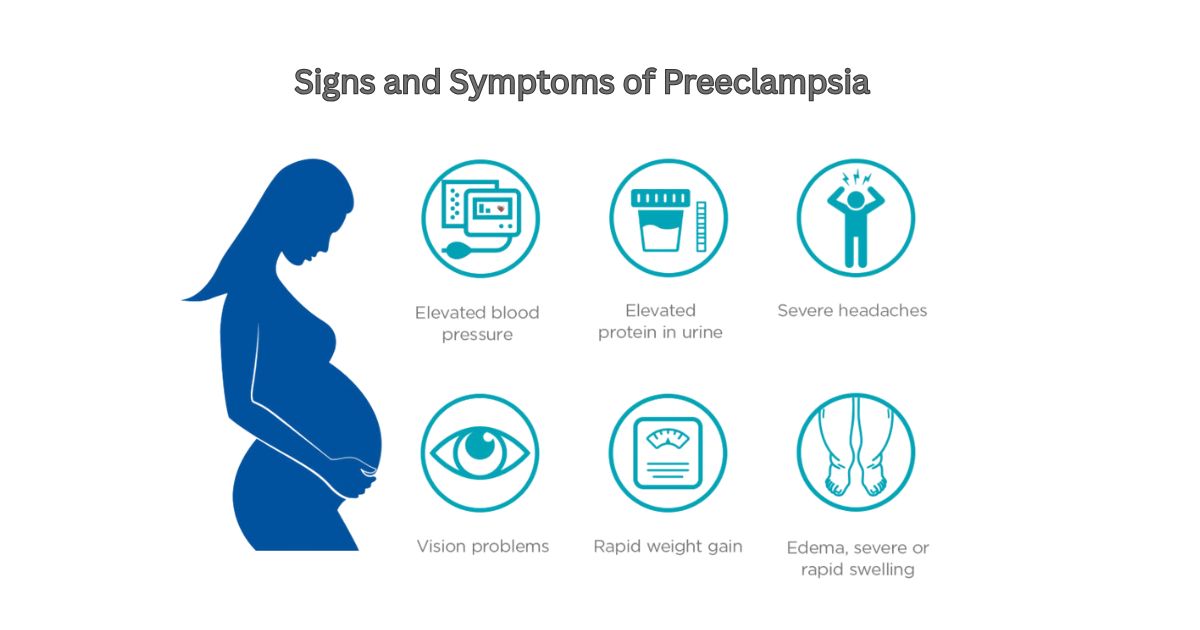
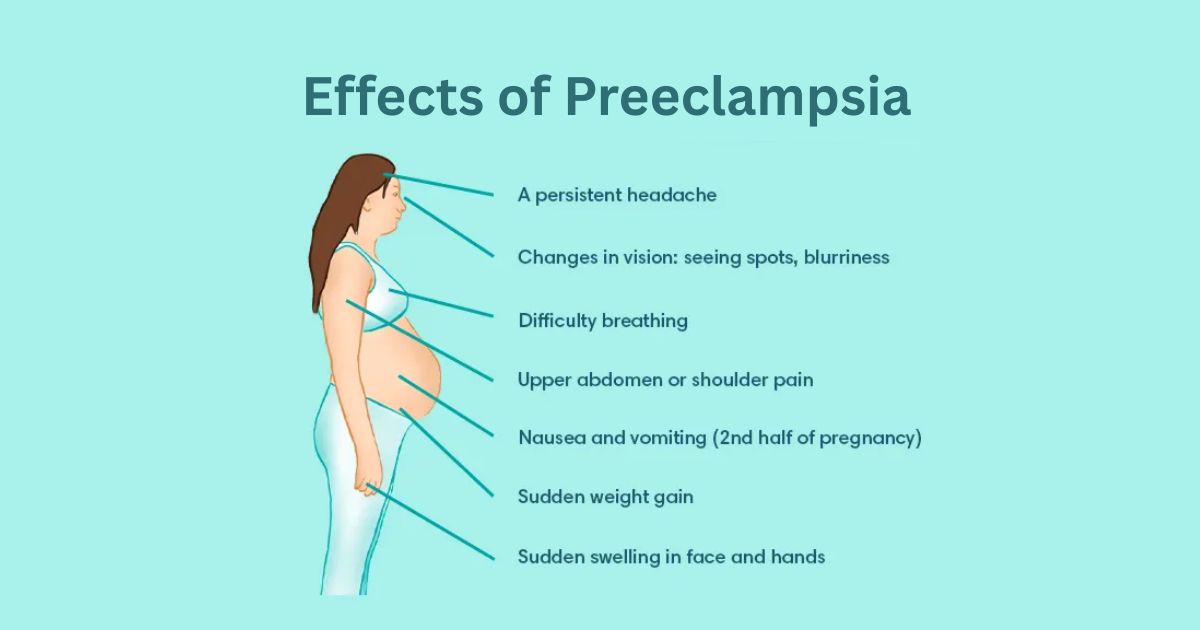
Preeclampsia refers to high blood pressure that occurs past 20th week of pregnancy and is usually accompanied by presence of protein in the urine or damage of organs. Its symptoms consist of persistent headaches, swelling of the hands and face, sight problems and sudden weight gain. Although mild cases can be contained, severe cases can pose a risk to the lives of the mother and the child. Indeed, preeclampsia has been one of the leading causes of maternal deaths in the world, and it has a strong association with endothelial dysfunction and malformed placental growth.
Is Preeclampsia Genetic or Environmental?
The inherited versus environmental driven debate on the subject of preeclampsia has long perplexed researchers. There is indication of a genetic pre-disposition to preeclampsia but the environment also influences results. Obesity, unhealthy eating habits, stress and access to medical care are lifestyle choices that play a big role in determining whether a person gets the condition. Nevertheless, research indicates that women with a positive family history of preeclampsia genetics have a high risk relative to no such history, indicating that the two factors may interact.
The Impact of Genetics on Risk of Preeclampsia
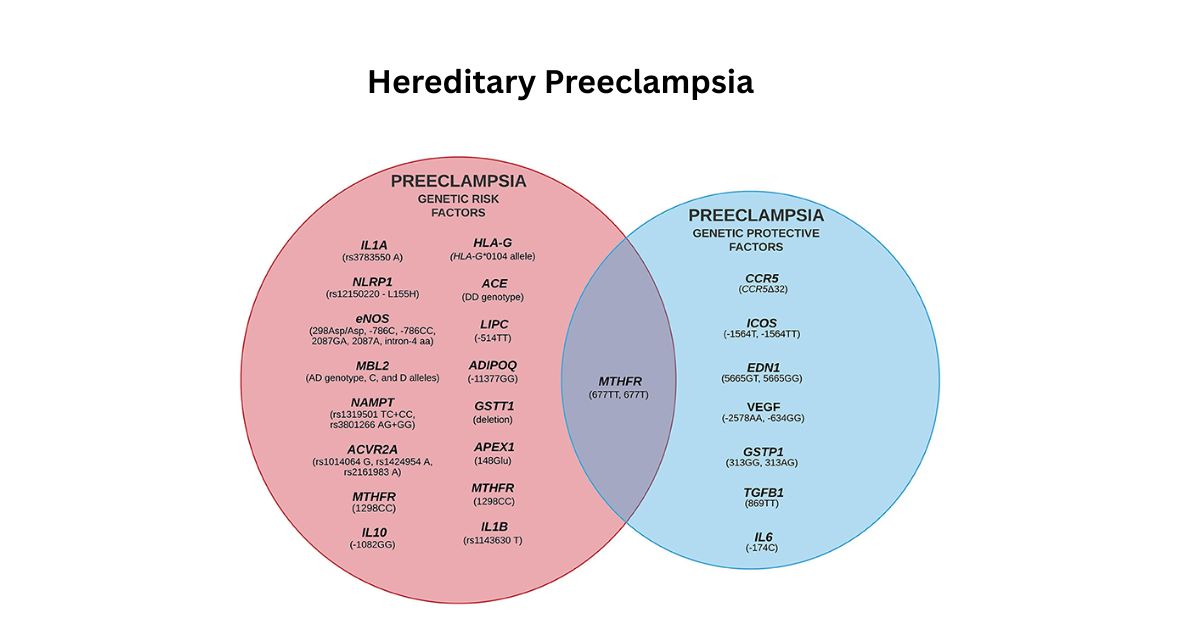
Scientists researching genetic association studies on preeclampsia found that one single mutation does not seem to increase the risk but instead a combination of several genes. These genetic variants of preeclampsia are distributed in the maternal and fetal genome. Others control the work of blood vessels, other ones the work of immunity, and others affect the placenta. Genome-wide screening and linkage research indicates that approximately 3050 per cent of the risk of preeclampsia can be inherited. That was the number to emphasize the level to which genes and gene expression regulation are the contributors to the pathophysiology of the disease.
Vascular Genes and Blood Vessel Functioning
The largest influence is provided by genes that control blood vessels. The angiogenic factors such as VEGF vary which dictates the expansion of blood vessels to deliver nutrients to the placenta. When such genes are mutated they can result into endothelial dysfunction, which results in high blood pressure and inadequate circulation during pregnancy. Such defective blood circulation is a significant symptom of preeclampsia.
Immune System Regulation
The other potent force is the genes that dictate the way the immune system reacts to the developing fetus. Under normal conditions, the body of the mother develops tolerance to the baby, but errors in genetic imprinting or certain polymorphisms may lead to an inflammation. Some candidate genes that have been associated in association studies as a cause of preeclampsia include HLA, which is involved in immune recognition.
Hereditary Predisposition and Family History
One of the best predictors of it is family history. In case your mother or your sister had developed it, you could be at risk between two and four times. Research on U.S. populations shows that a maternal genome contribution is critical, although fetal genome contribution is also important. To illustrate, the genes passed on by the baby can have a direct influence on the placenta development. This emphasizes the reason why scientists explain that it is a multifaceted genetic disease and not a single-cause disease.
Hereditary Preeclampsia
ERAP1, ERAP2 and VEGF are some of the genes linked with preeclampsia. These are engaged in blood pressure regulation, angiogenic factors and immune function. Association studies have detected mutations (or polymorphism) in these candidate genes. They affect the growth of the blood vessels and the tolerance of the immune system of the mother towards the fetus. These findings do not only describe the genetic disposition of preeclampsia, but also provide avenues to new therapies.
| Influence | Genes / Factors | Effect |
| Blood Vessels | VEGF, FLT1 | Abnormal growth leads to endothelial dysfunction. |
| Immune System | HLA, TNFSF13B | Poor tolerance poor immune maladaptation. |
| Placenta | ERAP1, ERAP2 | Dysfunction -oxidative stress. |
| Maternal Genome | ACE, AGT | Increases the risk of blood pressure. |
| Fetal Genome | IGF2, imprinting genes | Overgrowth stresses mother. |
| Gene Interactions | Multiple loci | Complex risk-amplifying polymorphs. |
The Placenta and Genes Expression
Preeclampsia is in the center of the placenta. Poor blood circulation and oxidative stress are caused by abnormal placental development and harm maternal organs. The regulation of genes that control the placenta demonstrates that there is an abnormal regulation of gene expression, which disrupts the oxygen and nutrient supply. The placenta can be imagined as the command center of pregnancy, when its orders are not properly followed, both the mother and the baby are in danger. Most scientists are of the opinion that the maternal and fetal genes have a balance that defines the effectiveness of the placenta functioning.
Maternity vs. Paternity Genetic contribution
The role of the DNA of both parents remains one of the most interesting in the genetics of preeclampsia. The maternal vs. fetal genes in preeclampsia bring out a tug of war in the womb. Although the genes of the mother play a role in the regulation of blood pressure and immune adaptation, it is possible that the genetic imprinting of the father may induce the growth of the placenta aggressively. This imprinting effect implies that even the paternal genetics can make a person more likely to develop preeclampsia which seems to be a shocking turn to a lot of families.
Interplay Between Gene and Environmental Factors in Preeclampsia
There is more to it than genes. It is an interaction of genes with environmental factors. Some high-risk its genes that a woman carries might not allow a woman to develop the disorder when her environment is conducive. In contrast, the condition can be triggered by poor nutrition, obesity or chronic high blood pressure in women who are genetically predisposed to it. There is a growing interest among researchers in the role of epigenetic alterations, or lifestyle-based modifications of the activity of the DNA, in connecting environmental stress to the alteration of the activation of harmful genetic pathways.
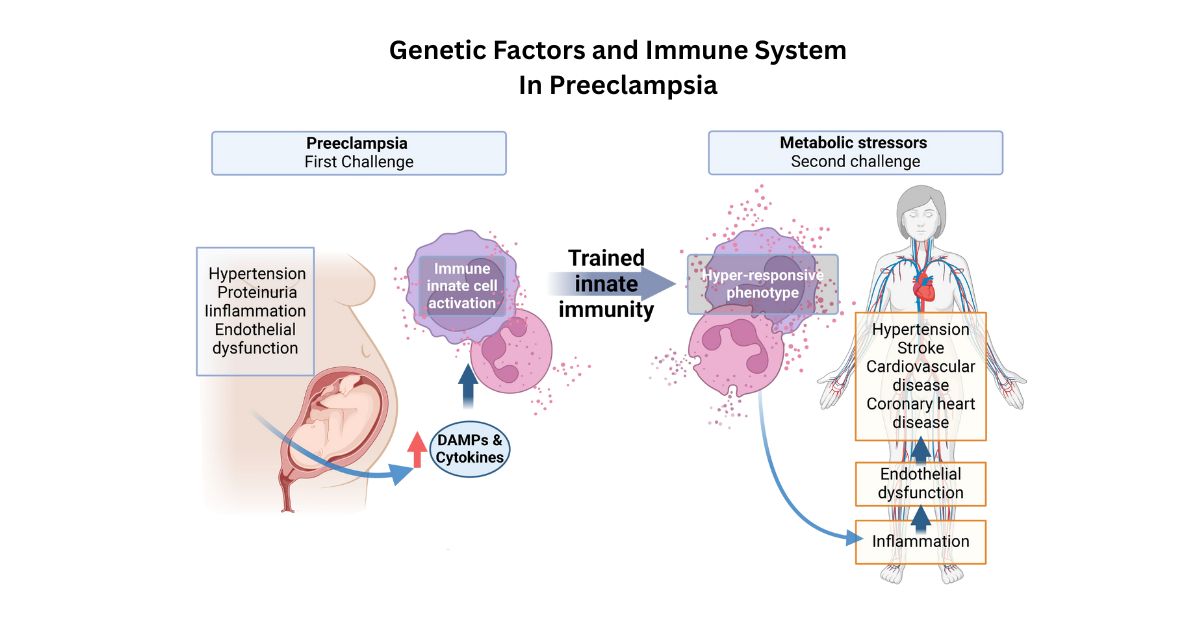
Genetic Factors and Immune System
It can be said to be an immunological mal-adaptation disease. A mother is supposed to have an immune system that should accept her baby as being partially foreign and yet not reject it. In preeclampsia, this tolerance is not successful due to some genetic imprinting errors and interactions of genes with each other. As an illustration, differences in human leukocyte antigen (HLA) genes, which are patrilineal in nature can trigger immune assaults on placenta. This is the same overlap of the immune action and the genes that relate to it as a result of which women with autoimmune disorders like lupus are more susceptible.
Will Genetic Tests Forecast Preeclampsia?
Currently, there is no universal test that will give the certainty that you will develop preeclampsia. Genetic testing preeclampsia Researchers are experimenting with genetic testing preeclampsia using polygenic risk scores and genome wide association preeclampsia studies. These methods combine a combination of several of its genetic variants to approximate the risk. Though they are promising, they are not yet trustworthy enough to be used on a day to day basis. Nevertheless, there is an indication that in the future, with the help of genetic profiles, doctors can adjust the needs of expectant mothers to their individual risk.
Genetic Variants and Preeclampsia Recent Studies
It has recently come into the limelight of large-scale association studies and genome-wide screens. Indicatively, American scientists discovered some preeclampsia genetic variants associated with the oxidative stress and blood vessel functionality. In one case study article published in American Journal of Obstetrics and Gynecology, it was demonstrated that women carrying some specific ERAP2 variants were found to have much higher incidences of preeclampsia. These and similar results validate the importance of genome wide association in studies, but also indicate that numerous other factors are involved.
Prospects of Genetic Studies on Preeclampsia
Genetics and personalized medicine are the way to go in research in the future. Positional cloning breakthroughs, artificial intelligence, and massive biobank data are on the verge of figuring out the genetic blueprint of preeclampsia. In my opinion, genetic testing of preeclampsia will be customized and anticipatory in the future. Scientists believe that this will give rise to new therapies to address abnormal angiogenic factors or pathophysiology due to polymorphism. Predictive models could ultimately be used to incorporate family history, genetics and environment into a single risk score that can be beneficial to women.
Additional Risk Factors Not Genetic
Although genes do play a significant part, they are not the only factors. Mother age above 35, obesity, diabetes, chronic hypertension and multiple pregnancies are other risk factors. The CDC states that social and healthcare disparities mean that African American women are 60% more likely to get preeclampsia than white women. The impacts of genetic vulnerability can be exacerbated by these factors to form strata of risk that need to be considered jointly.
Is it Possible to Prevent Preeclampsia When you are at Risk because of your Genetic Background?
Although you cannot modify your DNA, you can play down the risk. Women whose family has a history of the preeclampsia heredity may also have advantages of early prenatal care, routine blood pressure monitoring and low-dose aspirin prescribed by the doctor in some instances. I believe that such a simple change as a healthy diet and stress management usually helps a lot. The information about your genomic predisposition to preeclampsia may prompt better lifestyle behaviors including better diet, physical activity, and stress management. It is not a foolproof method of prevention, but the effects of genetic susceptibility can be lessened by taking pro-active measures.
Conclusion
So, is preeclampsia genetic? The fact is yes, but not completely. It can best be seen as a result of inherited genes as well as environmental factors. DNA of the mother and father, the placenta, as well as the external lifestyle choices, combine in a complicated pattern. Next-generation advances in genetic testing preeclampsia will one day hopefully enable us to predict and even prevent it with even more accuracy. At this time, the best means of maintaining a safe mother and baby are their awareness, family history, and medical care.
FAQs
Is preeclampsia a maternal or paternal inherited disease?
Yes there is a contribution of both the maternal and paternal genes, but when it comes to causing family history the maternal side is more associated.
Which genes have something to do with preeclampsia?
ERAP1, ERAP2, and VEGF genes, which control blood pressure and immune reaction, have been associated with preeclampsia.
Is it possible to predict the risk of preeclampsia by genetic testing?
Genetic preeclampsia testing is not as a standard yet but polygenic risk scores are promising in research studies.
What are the risk factors of preeclampsia other than genetics?
Risk factors, including age, obesity, diabetes, multiple pregnancies, and race are also at risk in addition to genetic predisposition.
Is it possible to prevent preeclampsia in case it is a family matter?
Although it cannot be completely avoided, early prenatal care, lifestyle changes and in certain instances low-dose aspirin can have beneficial effects.

 Medically reviewed by
Medically reviewed by