What is Lacunar Stroke?
A lacunar stroke is a small, deep ischemic infarct, typically less than 15 mm, caused by blockage of a tiny penetrating artery supplying the brain’s deep structures. These perforating vessels feed critical regions such as the internal capsule, thalamus, basal ganglia, and pons, which is why even a small clot can cause sharply defined neurological deficits. Clinically, the pattern is highly consistent: sudden, focal problems without the cortical features like aphasia or visual field loss seen in other stroke types.
Difference Between Lacunar, Silent, and Other Small Vessel Strokes
Understanding how lacunar strokes differ from other stroke types is essential for diagnosis, management and prognosis.
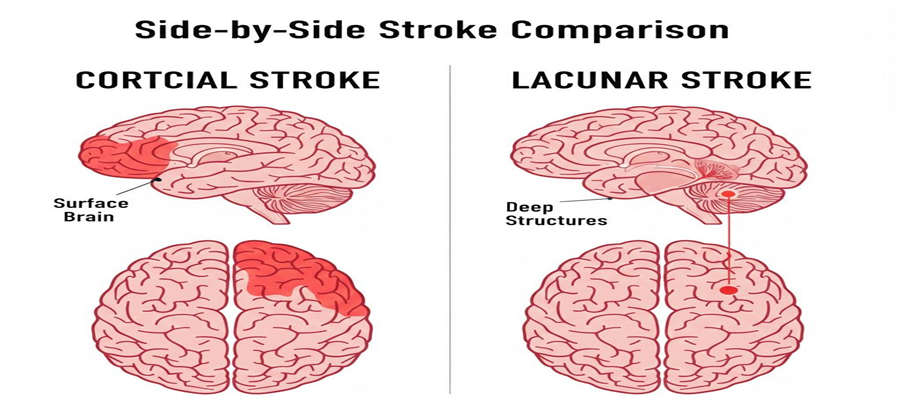
Lacunar Stroke vs Cortical Stroke
- Cortical strokes: Involve the outer layers of the brain, usually due to large-vessel atherothrombosis or cardio embolism. Present with cortical signs such as aphasia, visual field deficits, neglect, or gaze preference.
- Lacunar strokes: Spare the cortex, causing only deep, focal deficits.
Lacunar Stroke vs Silent Stroke
- Silent lacunes: Detected on imaging without noticeable stroke symptoms.
- Symptomatic lacunar strokes: Present with classic lacunar syndromes such as pure motor hemiparesis, pure sensory stroke, dysarthria–clumsy hand, or ataxic hemiparesis.
Both reflect small-vessel disease, but silent lacunes are often incidentally discovered on MRI. Despite being asymptomatic, they still carry long-term cognitive and vascular risk.
Lacunar Stroke vs Watershed Stroke
- Lacunar strokes: Tiny, deep subcortical infarcts caused by small-vessel disease affecting perforating arteries. Produce deep, focal deficits without cortical signs.
- Watershed strokes: Occur at the border zones between major cortical arteries (cortical or white-matter junctions), usually triggered by systemic hypoperfusion or embolic events. Clinically, they cause diffuse weakness or cognitive deficits rather than isolated focal syndromes.
Key difference: Lacunar strokes are highly stereotyped and focal, whereas watershed strokes are more diffuse and often linked to systemic events.
Why Does it Represent Small Vessel Disease?
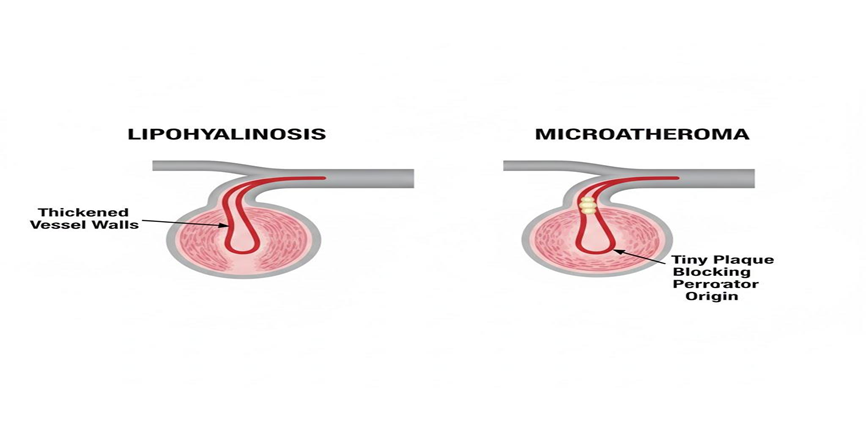
Lacunar strokes are considered the hallmark of cerebral small vessel disease (SVD). The root cause is not a large clot but chronic damage to small penetrating arteries. Key mechanisms include:
Lipohyalinosis: Long-standing hypertension thickens and degenerates vessel walls, eventually causing blockage.
Microatheroma: Tiny atherosclerotic plaques develop at the origin of perforating arteries, narrowing the lumen and reducing blood flow.
Typical Age Group and At-Risk Populations
Lacunar strokes can occur in adults of almost any age, but they are most common in middle-aged and older adults, particularly those with risk profiles characteristic of cerebral small vessel disease. The two dominant risk factors are:
- Longstanding hypertension: The strongest driver of perforating artery damage.
- Diabetes mellitus: Accelerates microvascular degeneration and worsens outcomes.
Other high-risk groups include individuals with metabolic syndrome, chronic kidney disease, or poorly controlled vascular risk factors. Clinicians can often identify vulnerable patients years before imaging detects a lacunar, as chronic elevation of blood pressure and blood sugar silently damages the brain’s tiniest vessels.
Mechanisms: Lipohyalinosis vs Microatheroma
Lipohyalinosis
- Chronic hypertension damages the vessel wall, causing fibrous thickening, degeneration, and eventual lumen collapse.
- This is the textbook mechanism of small vessel disease and is the predominant cause in patients with long-standing high blood pressure.
Microatheroma
- Tiny atherosclerotic plaques form at the origin of perforating arteries.
- These miniature plaques may not be obvious on imaging but are sufficient to block blood flow to deep brain regions.
Clinicopathologic studies confirm that lacunar infarcts consistently map to these mechanisms, reflecting years of silent microvascular injury rather than random events.
Common Brain Regions Affected
Lacunes occur in predictable locations because certain perforating arteries are especially vulnerable. The most frequently affected regions include:
- Posterior limb of the internal capsule: Small infarcts here can disrupt descending motor fibers, causing pure motor hemiparesis.
- Corona radiata: Infarcts may produce mixed motor and sensory symptoms.
- Basal ganglia (especially the putamen): Dense circuits make this a hotspot for small-vessel occlusion.
- Thalamus: Concentrated sensory pathways often result in pure sensory strokes.
- Pons: Pontine perforators cause classic syndromes such as ataxic hemiparesis.
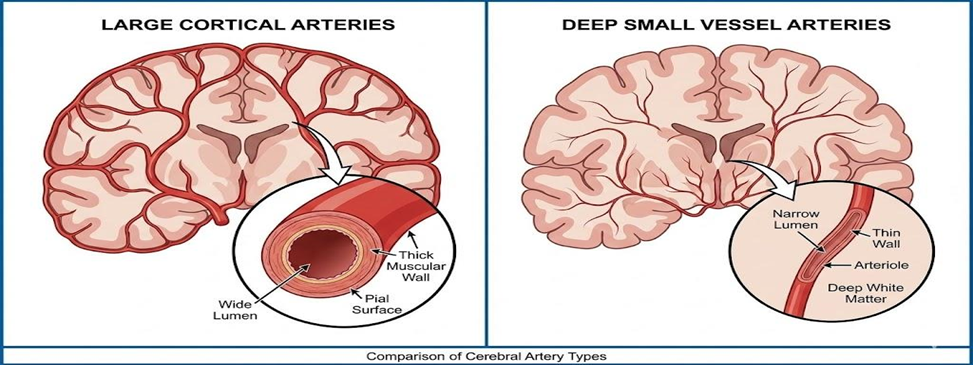
Small Perforating Arteries Involved
The hallmark of lacunar stroke pathophysiology lies in the tiny perforating arteries branching from major cerebral vessels to feed deep brain structures. These small vessels supply:
- Basal ganglia
- Thalamus
- Internal capsule
- Deep white matter
Because these arteries lack collateral support, even a microscopic blockage can produce a sharply defined infarct. The deep penetration of these vessels makes them particularly vulnerable to chronic microvascular injury.
Causes and Risk Factors
Understanding the causes and risk factors of lacunar stroke is critical, as most of these are modifiable.
1. Hypertension: The Primary Driver
Chronic high blood pressure is the no 1 cause of lacunar strokes. Persistently elevated blood pressure damages small penetrating arteries, leading to:
- Thickened and stiffened vessel walls
- Narrowed lumens that restrict blood flow
Patients with long-standing or uncontrolled hypertension are far more likely to develop lacunar infarcts and experience worse outcomes.
2. Diabetes and Metabolic Syndrome
Diabetes mellitus accelerates small-vessel damage through chronic inflammation and glycation. Over time, this:
- Increases the risk of lacunar stroke
- Worsens post-stroke disability
When combined with obesity, high triglycerides, or insulin resistance (components of metabolic syndrome), the risk multiplies, making these patients particularly vulnerable to cerebral small vessel disease.
3. Smoking and Lifestyle Factors
Smoking contributes to endothelial injury, promotes clot formation, and accelerates small-vessel degeneration, all of which predispose to lacunar stroke. Additional lifestyle risks include:
- Dyslipidemia (high LDL, low HDL)
- Sedentary lifestyle
These factors act synergistically, compounding the risk to perforating arteries over time.
4. Other Vascular Diseases
Not all small deep strokes are classic lacunar infarcts. Other potential causes include:
- Parent artery atherosclerotic plaques obstructing the origin of a perforator.
- Tiny emboli from the heart or large arteries lodging in deep brain territories.
Identifying these cases is important, as different causes require different treatments and influence long-term management strategies.

Clinical Features of Lacunar Stroke
Classic Lacunar Syndromes
There are five stereotyped presentations you must know:
- Pure Motor Hemiparesis – lesions in the internal capsule or basis pontis, causing isolated weakness on one side of the body.
- Pure Sensory Stroke – thalamic lesions leading to isolated numbness or sensory deficits.
- Sensorimotor Stroke – involvement of the thalamocapsular region, producing combined motor and sensory impairment.
- Dysarthria–Clumsy Hand Syndrome – lesions in the pons or internal capsule, leading to slurred speech and hand clumsiness.
- Ataxic Hemiparesis – affecting the pons or corona radiata, combining weakness with coordination problems.
Subtle or Atypical Presentations
Not all lacunar strokes are dramatic. Some are tiny, deep, and deceptive, presenting with:
- Mild weakness or numbness
- Fluctuating or vague symptoms
- White-matter lacuna’s that appear inconsequential until deficits accumulate
This subtlety is why many lacunar strokes are overlooked or diagnosed late, especially if clinicians rely solely on early imaging.
Why are Lacunar Strokes Hard to Spot?
Lacunar infarcts are small and buried deep in the brain, which makes early detection challenging:
- CT Scan: Often misses acute lacunes in the first hours.
- Conventional MRI (without DWI): Can be unreliable for tiny lesions.
- Diffusion-Weighted Imaging (DWI) MRI: The most reliable tool for detecting acute lacunar strokes, but even then, clinical recognition of classic syndromes remains essential.
Diagnosis
CT vs. MRI – Which Detects Lacunar Infarcts Better?
Non-contrast CT: Not reliable for acute lacunar strokes. Lesions are tiny and deep, so CT mainly serves to rule out haemorrhage rather than confirm a lacunae.
Importance of Diffusion-Weighted MRI
Diffusion-Weighted Imaging (DWI) MRI: The preferred modality. DWI identifies acute lacunar infarcts with ~90–95% sensitivity and can distinguish acute vs chronic lesions using ADC patterns
ADC (Apparent Diffusion Coefficient) measures water movement in brain tissue on MRI.
Tip: If DWI isn’t used, small lacunar strokes can easily be missed, delaying treatment.
Ruling Out Cortical Stroke and Haemorrhage
Before diagnosing a small-vessel lacune, clinicians must exclude:
- Cortical ischemia
- Intracranial haemorrhage
Standard diagnostic workflow:
- Non-contrast CT: Immediate scan to exclude bleeding, especially before thrombolysis.
- MRI (DWI) and vascular imaging: Confirms lacunar infarct patterns and ensures deficits aren’t caused by cortical stroke or parent-artery occlusion.
Laboratory Workup and Risk Assessment
To guide secondary prevention and rule out alternative causes, labs and imaging should cover vascular risk and embolic sources:
- Blood tests: Glucose, CBC, renal function, coagulation profile (if needed).
- Cardiac evaluation: ECG ± echocardiography to rule out atrial fibrillation or cardio embolism.
- Vascular imaging: CTA, MRA, or carotid Doppler to exclude large-artery atherosclerosis.
Treatment
Management of lacunar stroke combines standard acute ischemic stroke protocols with specific strategies tailored to small-vessel infarcts.
Acute Care Protocols
Immediate priorities in the emergency setting include:
- Rapid triage to identify stroke symptoms.
- Non-contrast CT scan to rule out haemorrhage.
- IV thrombolysis (tPA) consideration if within the treatment window and deficits are disabling.
- Time is brain: Even though lacunes are small, early intervention prevents progression and reduces complications.
Thrombolysis Eligibility (tPA Window)
Current guidelines permit IV-rt PA within 4.5 hours for eligible ischemic stroke patients. For lacunar strokes, eligibility depends on:
- Disabling vs. non-disabling deficits.
- aAbsence of contraindications such as recent surgery, haemorrhagic risk, or coagulopathy.
Blood Pressure and Glucose Control
Careful management of blood pressure and glucose is essential during the acute phase:
- Blood pressure: Avoid rapid lowering before tPA unless systolic or diastolic values are dangerously high.
- Glucose: Normalize hyperglycemia to reduce neuronal injury.
Long-term, strict blood pressure control is critical to reduce recurrence risk. Trials such as SPS3 (Secondary Prevention of Small Subcortical Strokes)support targeting lower systolic blood pressure in patients with lacunar strokes for improved outcomes.
Antiplatelet Therapy and Secondary Prevention
For non-cardioembolic lacunar strokes:
- Single antiplatelet therapy (usually aspirin) is standard for long-term prevention.
- Short-term dual therapy (aspirin + clopidogrel) may be used for minor stroke or TIA, typically limited to 21 days.
- Long-term dual therapy is harmful, increasing bleeding risk without lowering recurrence, as shown in the SPS3 trial.
Recovery and Prognosis
The prognosis of lacunar stroke varies depending on lesion size, location, and control of vascular risk factors.
Short-Term Recovery
Many patients experience rapid motor improvement within the first days to weeks, especially with small infarcts. However, recovery depends heavily on lesion location:
- Infarcts in the posterior limb of the internal capsule may leave persistent motor weakness despite therapy.
- Early physical and occupational rehabilitation significantly improves functional outcomes.
Long-Term Outcomes
Compared to large-vessel or cortical strokes, lacunar strokes usually have better long-term function.
Repeated lacunar events or widespread small-vessel disease can accumulate over time, causing:
- Progressive disability
- Gait impairment
- Reduced independence
Continuous vascular risk management controlling blood pressure, diabetes, and cholesterol is crucial to preserving function.
Recurrence Risk
The likelihood of a recurrent lacunar stroke strongly correlates with vascular risk factor control. Evidence from the SPS3 trial and other studies identifies predictors of recurrence:
- High systolic blood pressure
- Diabetes mellitus
- Renal dysfunction
- Low hemoglobin
Cognitive Effects: The Lacunar State
Multiple lacunes and extensive small-vessel disease can cause vascular cognitive impairment, sometimes progressing to subcortical ischemic vascular dementia, also known as the “lacunar state.” Features include:
- Slow processing speed
- Executive dysfunction
- Memory decline
- Gait disturbance
Prevention
Controlling Hypertension
Hypertension is the single most important modifiable risk factor for lacunar stroke. Clinical trials show that tightly controlling systolic blood pressure (SBP) significantly reduces the risk of recurrence.
- Target lower SBP values when safely tolerated to protect small vessel health.
- Consistent blood pressure control slows progression of cerebral small vessel disease.
Managing Diabetes and Metabolic Syndrome
Persistent hyperglycemia accelerates microvascular damage, increasing the risk of lacunar infarcts. Effective management strategies include:
- Optimizing blood glucose levels.
- Treating components of metabolic syndrome such as obesity, dyslipidemia, and hypertension.
Lifestyle Interventions
Healthy lifestyle choices play a major role in primary and secondary prevention:
- Smoking cessation: Prevents endothelial injury and reduces clot formation.
- Regular exercise: Enhances vascular resilience and blood flow.
- Balanced diet and lipid control: Minimizes systemic atherosclerosis.
Complications of Lacunar Stroke
Even though lacunar strokes are small, they can cause significant long-term complications affecting motor, cognitive, and emotional function.
Motor and Sensory Disabilities
Small lacunar infarcts can leave persistent deficits depending on lesion location:
- Posterior limb of the internal capsule: Often results in lasting motor weakness.
- Thalamus or corona radiata: May produce sensory loss or subtle coordination problems.
Vascular Dementia and Cognitive Decline
Repeated lacunes and extensive white-matter small-vessel disease are strongly associated with vascular cognitive impairment. Patients may develop:
- Progressive memory difficulties
- Executive function deficits
- Gait disturbances
Emotional and Behavioral Changes
Subcortical strokes frequently cause post-stroke depression, emotional lability, and apathy. These issues can impact:
- Rehabilitation adherence
- Overall recovery
- Quality of life
Case Example: Mapping Syndromes to Lesions in Lacunar Stroke
Patient Presentation
A 62-year-old man with a long history of hypertension and type 2 diabetes presented with a sudden onset of right-sided weakness. On neurological examination, he was found to have pure motor hemiparesis affecting the right arm and leg, without any accompanying sensory loss, aphasia, visual changes, or other cortical signs. This constellation of symptoms strongly suggested a classic lacunar syndrome, most consistent with a lesion in the deep motor pathways.
Management Decisions
The patient arrived within the 4.5-hour therapeutic window for intravenous thrombolysis, and because his motor deficit was considered moderate but clearly disabling, IV tPA was administered safely. Blood pressure was managed cautiously to maintain adequate cerebral perfusion while reducing the risk of haemorrhagic transformation. For secondary prevention, the patient was started on single antiplatelet therapy with aspirin, along with strict blood pressure and glucose control. He also received lifestyle counseling and statin therapy as part of long-term vascular risk reduction.
Outcome and Follow-Up
The patient demonstrated substantial motor improvement over the course of four weeks with structured physiotherapy. During long-term follow-up, emphasis was placed on rigorous management of vascular risk factors to reduce the likelihood of recurrent stroke. This case reinforces key lessons including the strong correlation between pure motor hemiparesis and posterior internal capsule involvement, the value of DWI MRI in identifying small-vessel strokes, and the importance of evidence-based acute and secondary prevention strategies.
When to Seek Medical Advice?
If you or someone around you suddenly develops weakness, numbness, slurred speech, imbalance, or sudden confusion, don’t wait seek emergency care immediately. Lacunar strokes are small, but the damage isn’t. Early evaluation helps determine tPA eligibility, imaging needs, and targeted rehabilitation.
For those already diagnosed, schedule regular follow-ups with a neurologist to review blood pressure control, diabetes management, antiplatelet therapy, and long-term recovery plans.

 Medically reviewed by
Medically reviewed by