Women often struggle for years with menstrual problems, hormonal changes, weight gain, infertility and chronic pelvic pain. Two of the most common conditions linked with these symptoms are Polycystic Ovary Syndrome (PCOS) and Endometriosis. Although both affect reproductive health, they are completely different in nature. Misunderstanding between these two conditions often delays diagnosis. This blog explains PCOS vs Endometriosis, their signs, symptoms, causes, diagnosis, treatment and lifestyle strategies.
Learning About PCOS (Polycystic Ovary Syndrome)
PCOS is a hormonal disorder which is brought about by a disproportion of female hormones. Androgens are increased in women with PCOS, and this interferes with ovulation. The result of this imbalance is irregular periods, infertility, acne, hair growth (hirsutism) and weight gain. PCOS is commonly experienced when one is in the teenage years, yet most women are diagnosed when they are in their reproductive years.
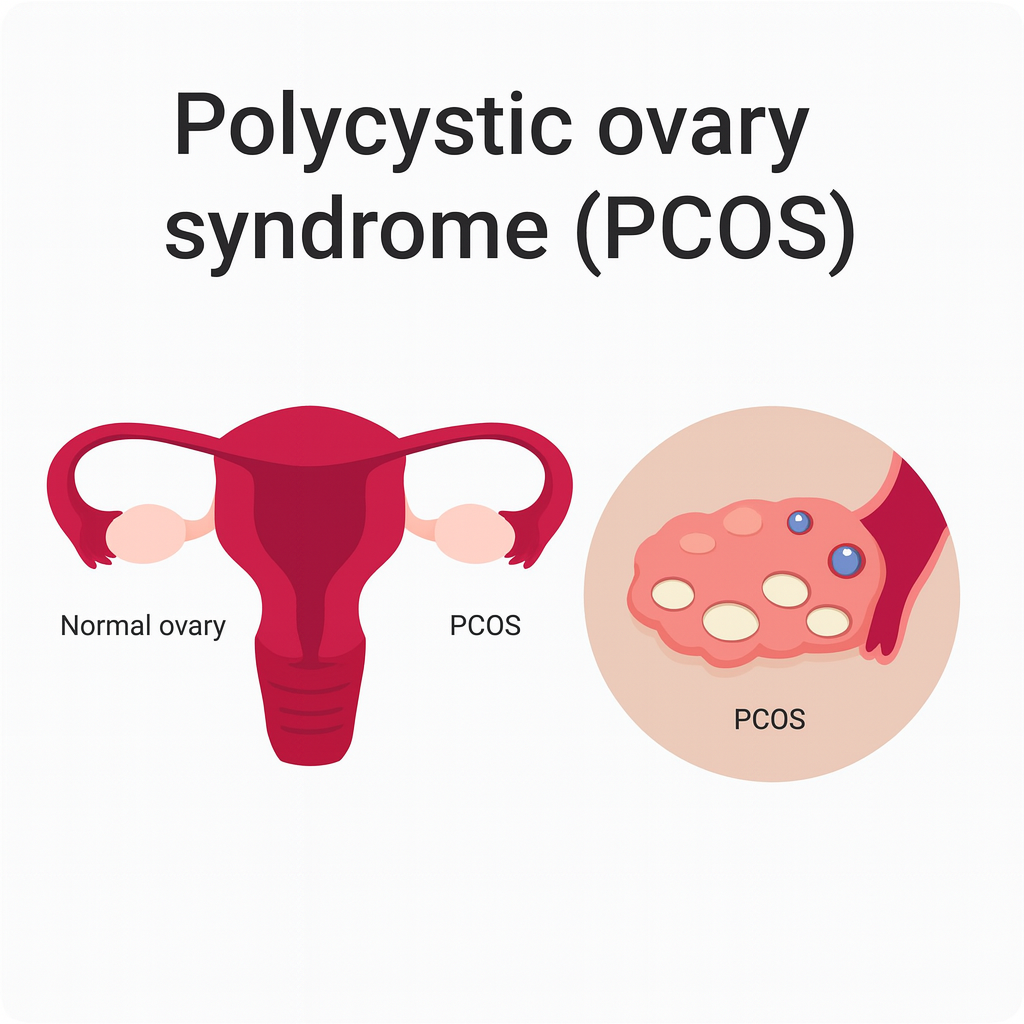
The hormonal variations disrupt the growth of ovarian follicles. Rather than owing to the regular release of eggs, several small follicles envelop the ovaries. These are usually known as polycystic ovaries, but cysts are not necessarily damaging. PCOS is an incurable disorder, yet symptoms may be managed through adequate dietary, physical and drug interventions.
Knowing Endometriosis and Pelvic Pain
Make-A-Wish Endometriosis is a disorder, which the tissue, which is like the uterine lining, develops outside the uterus. This displaced tissue is hormone responsive every month. It becomes thick, decays and haemorrhages, yet the blood is not able to leave the body. This leads to inflammation, chronic pelvic pains, painful periods, cysts and adhesions.
Endometriosis is not a hormonal condition as compared to PCOS. It is regarded as an estrogen-dependent disease and an inflammatory disease. It may include ovaries, fallopian tubes, bladder, bowel and pelvic walls, resulting in excruciating pain during menstrual periods and intercourse.
PCOS vs Endometriosis: Major Differences in a Nutshell
Polycystic Ovary Syndrome (PCOS) is mainly a hormonal and metabolic disorder, whereas endometriosis is a chronic inflammatory condition that is estrogen dependent. PCOS primarily affects ovulation, insulin regulation, and androgen levels, while endometriosis involves the growth of endometrial-like tissue outside the uterus, leading to inflammation and scarring.
Women with PCOS commonly experience irregular or absent menstrual cycles, acne, excessive hair growth, and weight changes due to hormonal imbalance. In contrast, endometriosis is typically marked by severe menstrual cramps, chronic pelvic pain, painful intercourse, and discomfort during bowel movements.
Aetiology and Predisposing Factors to PCOS
PCOS is a multifactorial condition with contributions from genetic predisposition, hormonal imbalance, and environmental influences, although its exact cause remains incompletely understood.
- Insulin resistance plays a central role in PCOS, leading to elevated insulin levels that stimulate the ovaries to produce excess androgens.
- A positive family history increases the likelihood of developing PCOS, indicating a hereditary component.
- Sedentary lifestyle, poor dietary patterns, and obesity exacerbate insulin resistance and increase the risk and severity of PCOS.
- Chronic low-grade inflammation is believed to contribute to PCOS by promoting androgen secretion from the ovaries.
- Excess androgen production disrupts normal ovulation, resulting in irregular or absent menstrual cycles.
- Hormonal dysregulation associated with PCOS often leads to subfertility or infertility.
Aetiology and Risk Factors of Endometriosis
- Retrograde menstruation is one of the most widely accepted mechanisms, where menstrual blood flows backward into the pelvic cavity, allowing endometrial-like cells to implant outside the uterus.
- Genetic predisposition increases susceptibility, with higher risk observed in women who have first-degree relatives affected by endometriosis.
- Immune system dysfunction may impair the clearance of ectopic endometrial tissue, facilitating its persistence and progression.
- Environmental factors, including exposure to endocrine-disrupting chemicals, are believed to contribute to disease development.
- Early onset of menstruation (early menarche) is associated with an increased risk of endometriosis.
- Short menstrual cycles and heavy or prolonged menstrual bleeding elevate the likelihood of disease occurrence.
- Endometriosis is strongly linked to estrogen dependence and chronic inflammation.
- Unlike PCOS, endometriosis shows no consistent association with obesity or insulin resistance.
Symptoms of PCOS
- Irregular, infrequent, or absent menstrual cycles are among the most common presenting features.
- Excess androgen levels may cause hirsutism (excess facial or body hair), acne, and thinning of scalp hair.
- Weight gain, particularly central or abdominal obesity, is frequently observed.
- Anovulation or irregular ovulation often leads to difficulty conceiving and infertility.
- Beyond reproductive symptoms, PCOS can affect overall health and well-being.
- Women with PCOS may experience fatigue, mood disturbances, anxiety or depression, and sleep disorders.
- PCOS increases the risk of metabolic syndrome, including insulin resistance.
- Long-term complications include type 2 diabetes mellitus, hypertension, and dyslipidemia.
- Prolonged unopposed estrogen exposure may lead to endometrial hyperplasia and increased endometrial cancer risk.
Symptoms of Endometriosis
- Severe dysmenorrhea is a common and often early symptom.
- Chronic pelvic pain may persist throughout the menstrual cycle.
- Pain during sexual intercourse (dyspareunia) is frequently reported.
- Painful bowel movements, particularly during menstruation, can occur.
- Lower back or abdominal pain is commonly associated with the condition.
- Some women experience heavy menstrual bleeding, prolonged periods, or irregular spotting.
- Bloating, nausea, and persistent fatigue are additional non-specific symptoms.
- Infertility is a significant complication due to inflammation, adhesions, and scarring affecting the ovaries and fallopian tubes.
- Chronic pain and delayed diagnosis often lead to psychological distress, anxiety, and depression, negatively impacting quality of life.
Diagnosis
PCOS
The diagnosis of Polycystic Ovary Syndrome is primarily clinical, supported by laboratory and imaging findings. It is commonly based on the Rotterdam criteria, which require the presence of at least two of the following three features after excluding other endocrine disorders: irregular or absent ovulation, clinical or biochemical signs of hyperandrogenism, and polycystic ovarian morphology on ultrasound. Blood tests are used to assess androgen levels, glucose and insulin status, lipid profile, and to rule out conditions such as thyroid dysfunction, hyperprolactinemia, and congenital adrenal hyperplasia. Pelvic ultrasound helps identify enlarged ovaries with multiple small follicles.
Endometriosis
The diagnosis of endometriosis is often challenging and delayed due to non-specific symptoms. It begins with a detailed clinical history and pelvic examination focused on chronic pelvic pain and menstrual symptoms. Transvaginal ultrasound may identify ovarian endometriomas or deep infiltrating disease but cannot reliably detect superficial lesions. MRI is useful for mapping deep or complex disease. The gold standard for definitive diagnosis remains laparoscopy with histological confirmation, which allows direct visualization and biopsy of endometrial-like tissue outside the uterus.
Treatment of PCOS
Lifestyle Modification
Lifestyle changes are the cornerstone of PCOS management and include weight reduction, regular physical activity, and a balanced diet to improve insulin sensitivity and hormonal regulation.
Hormonal Therapy
Combined oral contraceptive pills are commonly used to regulate menstrual cycles and reduce hyperandrogenic symptoms such as acne and hirsutism.
Insulin-Sensitizing Agents
Medications such as metformin are prescribed to improve insulin resistance, support ovulation, and reduce metabolic risks.
Fertility Treatment
For women planning pregnancy, ovulation induction with letrozole or clomiphene citrate is the first-line treatment, with assisted reproductive techniques used when necessary.
Long-Term Management
Ongoing monitoring is essential to prevent complications such as type 2 diabetes, cardiovascular disease, and endometrial hyperplasia.
Treatment of Endometriosis

Pain Management
Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to manage pelvic pain and dysmenorrhea.
Hormonal Suppression Therapy
Hormonal treatments, including combined oral contraceptives, progestins, and GnRH analogues, are used to suppress estrogen and slow disease progression.
Surgical Treatment
Laparoscopic excision or ablation of endometriotic lesions is indicated in moderate to severe cases or when medical therapy fails.
Fertility-Preserving Treatment
Surgical intervention and assisted reproductive techniques may be used to improve fertility outcomes in women wishing to conceive.
Long-Term Disease Management
Endometriosis requires a long-term, individualized approach due to its chronic and recurrent nature, often involving multidisciplinary care.
Nutrition Management in PCOS and Endometriosis
| Condition | Recommended Foods | Intake Quantity | Foods to Limit / Avoid | Notes |
|---|---|---|---|---|
| PCOS | – Whole grains (oats, quinoa, brown rice) – Lean proteins (chicken, fish, tofu, legumes) – Healthy fats (olive oil, avocado, nuts, seeds) – High-fiber vegetables (spinach, broccoli, kale) – Low-glycemic fruits (berries, apples, pears) | – 3–4 servings whole grains/day – 2–3 servings lean protein/day – 1–2 servings healthy fats/day – 3–5 servings vegetables/day – 2–3 servings fruits/day | – Refined carbs (white bread, pastries, sugary drinks) – Processed foods – Excess sugar and sweets – Trans fats | Emphasize balanced meals with low glycemic index, regular portion sizes, and adequate hydration. Small frequent meals can help manage blood sugar. |
| Endometriosis | – Omega-3 rich foods (salmon, sardines, flaxseed, chia seeds) – Anti-inflammatory vegetables (leafy greens, peppers, cruciferous veggies) – Fruits rich in antioxidants (berries, cherries, citrus) – Whole grains (brown rice, oats, barley) – Legumes and plant-based proteins | – 2–3 servings fatty fish/week – 3–5 servings vegetables/day – 2–3 servings fruits/day – 3–4 servings whole grains/day – 1–2 servings legumes/day | – Red and processed meats – Dairy (for sensitive individuals) – High-sugar foods and refined carbs – Alcohol and caffeine (may worsen symptoms) | Focus on anti-inflammatory diet to reduce prostaglandin production and pelvic pain. Consider supplementation with vitamin D, magnesium, and omega-3 fatty acids if needed. |
Conclusion
PCOS and endometriosis are unique but influential disorders that need to be made known, diagnosed early, and treated individually. Although PCOS is mainly a hormonal and metabolic condition, and endometriosis is an inflammatory gynaecological condition, both have a considerable impact on reproductive health and quality of life. The knowledge of what distinguishes PCOS and endometriosis will enable women to seek the necessary medical assistance and implement the best lifestyle practices. Women with PCOS or endometriosis may have healthy, full lives with proper diagnosis and full management.
FAQ’s
1. How does PCOS differ primarily from endometriosis?
PCOS is a hormonal and metabolic disease, whereas endometriosis is an inflammatory disease, which entails the growth of tissues outside of the uterus.
2. Is it possible that PCOS and endometriosis can co-exist?
Yes, some women may co-exist with both PCOS and endometriosis.
3. And which one is more painful, PCOS or endometriosis?
Endometriosis tends to result in worse and permanent pelvic pains than PCOS.
4. What are the impacts of PCOS and endometriosis on fertility?
PCOS influences fertility by interfering with ovulation, whereas endometriosis influences fertility by interfering with inflammation and scarring.
5. What are the methods of diagnosis of PCOS and endometriosis?
Hormone tests and ultrasound are used to diagnose PCOS, whereas imaging or laparoscopy can be used to diagnose endometriosis.

 Medically reviewed by
Medically reviewed by