Stage 4 endometriosis is the worst stage of the infection in which there is an extensive proliferation of endometrial tissue that develops deep adhesions, ovarian cysts and chronic inflammation. By this point, the condition has spread to various organs, which include the ovaries, fallopian tubes, bowel, bladder and even the deeper parts of the pelvis. The advanced endometriosis patients have high levels of pelvic pain, painful cycles, infertility and gastrointestinal issues. The symptoms, early diagnosis, surgery and lifestyle management are crucial to understanding how to improve the quality of life.
What is Endometriosis?
Endometriosis is a chronic gynecological disorder in which tissue similar to the endometrial lining of the uterus grows outside the uterine cavity. These ectopic implants commonly appear on the ovaries, fallopian tubes, pelvic peritoneum, and surrounding pelvic organs. Because the tissue responds to menstrual-cycle hormones, it can thicken, bleed, and cause inflammation, which leads to scarring, adhesions, cyst formation, pelvic pain, and potential infertility.
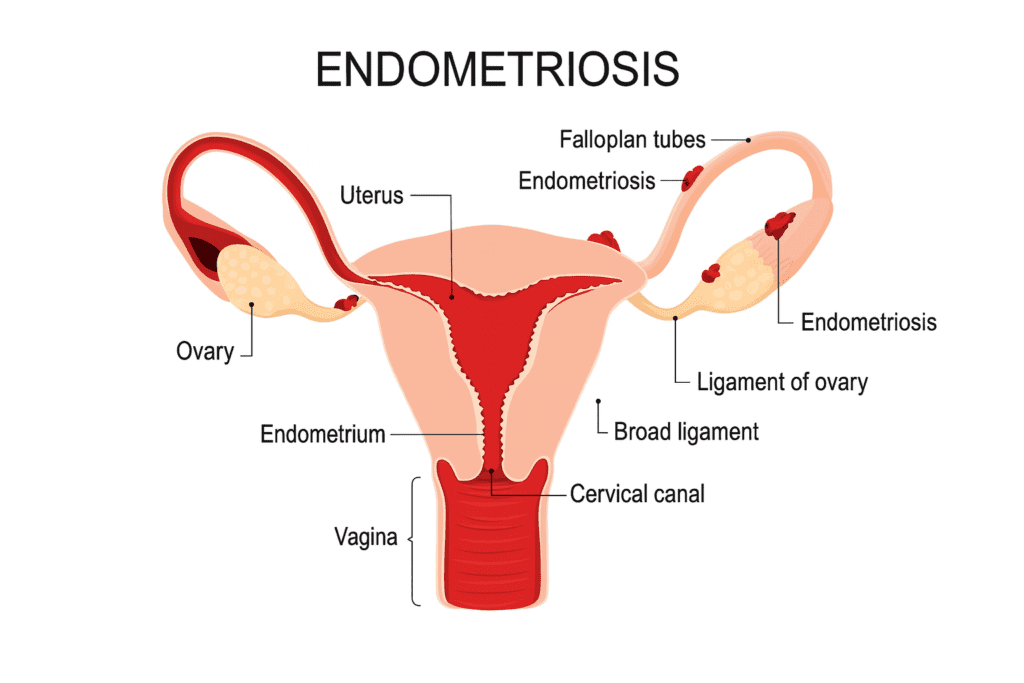
Endometriosis is categorized into four stages based on the extent, depth, and location of lesions, as well as the presence of adhesions and ovarian cysts:
- Stage 1 – Minimal Endometriosis
Small, superficial implants with minimal inflammation. Little to no scar tissue is present. - Stage 2 – Mild Endometriosis
More and deeper implants than Stage 1. Mild adhesions may begin to form. - Stage 3 – Moderate Endometriosis
Multiple deep implants with clear presence of adhesions. Small ovarian endometriomas (chocolate cysts) may be present. - Stage 4 – Severe Endometriosis
Extensive deep implants, large ovarian endometriomas, and thick, dense adhesions affecting multiple pelvic organs. This stage often causes significant pain and fertility challenges.
Learning About Stage 4 Endometriosis
Endometriosis stage 4, or deep infiltrating endometriosis, is a type of endometriosis that is diagnosed when the disease has proliferated to the extent that the organs are attached.
At this age, females normally possess big uterine endometriosis (chocolate cysts) on one or both ovaries. Adhesions can cause the organs to be out of their usual place, causing pain, infertility and bowel or bladder problems. This phase is commonly found in laparoscopy surgery, which is the gold standard diagnosis of endometriosis.
In Stage 4 Endometriosis Development: How it Arises?
Stage 4 is not an abrupt one. It evolves over a long period of time, usually due to the ignorance or misdiagnosis of symptoms. The endometrial implants also bleed every month. After a cyclical process, the body becomes scarred to repair the inflammation. With time, this scar tissue forms thick adhesions, which fix organs. Ovaries may be welded to the wall of the pelvis, the fallopian tubes may form twins, and the uterus may reach the bowel or bladder. This is excruciatingly painful and dysfunctional to the organs.
The chronic inflammation also boosts the development of painful cysts of old blood, referred to as endometriomas. Such cysts are usually 510 cm and cause painful movement and ovulation. Most stage 4 disease patients experience the symptoms not just during menstruation but at other times of the day.
Symptoms of Endometriosis at Stage 4
The symptoms at this age are severe. Severe pelvic pain is reported by most women, having an impact on their daily activities. Pain can be sharp, throbbing, burning or constant. The signs aggravate before periods, at the time of menstruation and ovulation. It is painful to the back, thighs and vaginal. There are those women who are unable to walk or stand during their periods.
Extremely painful periods (dysmenorrhea) are another symptom. The periods are thick, prolonged and clotty. The most common are nausea, vomiting, fainting and fatigue. A lot of patients are of the view that pain is normal, and they end up suffering in silence. However, period pain that halts daily functioning is not typical, and this is a significant indicator of severe endometriosis.
Painful intercourse (dyspareunia) is also a result of stage 4 disease. Scar tissue and adhesions cause internal organs to be drawn towards, thus, deep penetration is painful. Digestive symptoms are also common, particularly when the endometriosis is located in the rectum or the intestines. The females have constipation, diarrhoea, bloating and painful bowel movement. Symptoms of the bladder can be frequent urination, burning or pressure.
One of the most terrible consequences is infertility. The scar tissue blocks the fallopian tubes, does not release the eggs and interferes with the transportation of sperm normally. Approximately 30-50 per cent of women suffering from endometriosis have problems conceiving. Such physical and emotional problems render stage 4 endometriosis a challenge to live.
What is the Aetiology of Stage 4 Endometriosis?
No one cause exists, yet several theories have been used to explain the development of advanced endometriosis. The most acceptable theory is that of retrograde menstruation, where the menstrual blood is directed to flow backwards into the pelvis as opposed to leaving the body. This enables the pelvic organs to be implanted by endometrial cells.
There is also a strong influence of genetics. Endometriosis has a family history that is more dangerous in women. The growth of endometrial tissue is induced by hormonal imbalance, particularly high levels of oestrogen. The dysfunction of the immune system makes the body unable to remove cells that are out of place. The inflammation can be aggravated by lifestyle issues like chronic stress, improper diet, foods rich in fat and environmental toxins.
Diagnosis
Diagnosing Stage 4 endometriosis can be challenging because symptoms often overlap with other conditions such as irritable bowel syndrome (IBS), pelvic inflammatory disease (PID), or ovarian cysts. Many patients experience delays, with diagnosis commonly taking 7–10 years from the onset of symptoms. Physicians use several diagnostic tools to identify the disease:
1. Clinical Assessment
- Detailed medical history focusing on pelvic pain, menstrual irregularities, infertility, and gastrointestinal symptoms.
- Pelvic examination to detect tenderness, nodules, or fixed pelvic organs that may indicate adhesions or large endometriomas.
2. Imaging Studies
- Pelvic Ultrasound: Useful for detecting ovarian cysts (endometriomas) and assessing pelvic structures.
- Magnetic Resonance Imaging (MRI): Helps visualize deep infiltrating endometriosis, adhesions, and involvement of the bowel or bladder.
3. Minimally Invasive Evaluation (Gold Standard)
- Diagnostic Laparoscopy:
- A minimally invasive procedure in which a camera is inserted through small abdominal incisions.
- Allows direct visualization of lesions, adhesions, and endometriomas.
- Enables surgeons to biopsy tissue to confirm endometriosis.
- Treatment can be performed at the same time, such as removal of cysts and excision of lesions.
Treatment
Therapy varies based on the symptoms, next-gen fertility intention and disease severity. It is aimed at alleviating pain, managing inflammation, re-establishing organ performance and fertility.
Pain Management
Drugs used in pain relief are NSAIDs, heat, physiotherapy, acupuncture, and pelvic floor exercises. These are not a cure to the disease, but increase the quality of life, as well as decrease inflammation.
Hormonal Therapy
Hormones decrease estrogen and diminish the endometriosis lesions. They can be taken in the form of birth control pills, progestin therapy, GnRH analogues and hormonal IUD (Mirena). The treatments alleviate pain, excessive bleeding, but the illness can recur once the drug is stopped.
Stage 4 Endometriosis Surgery
In the case of advanced disease, surgery is the best remedy. Surgical laparoscopic excision enables surgeons to excise cysts, adhesions, as well as deep implants. It is possible to repair the normal structure of organs and enhance fertility through surgery. Some cases that have bowel or bladder severely impacted would require a section of the organ to be repaired.
In other women, a hysterectomy may be done when the pain becomes disabling, and fertility is not the priority anymore. Nevertheless, although surgical intervention is done, post-operative follow-up and lifestyle management are required to avoid recurrence.
Fertility Treatment
If a pregnancy is hard to conceive with natural methods, fertility specialists can suggest ovulation induction, IUI or IVF. The success rates of IVF are increased following endometriosis surgery due to the fact that the environment of the pelvis is healthier.
Complications at Stage 4
- Can lead to long-term health problems if untreated.
- Causes chronic pelvic pain affecting daily activities and overall quality of life.
- Dense adhesions may result in bowel obstruction or bladder dysfunction.
- Painful intercourse can negatively affect intimate relationships.
- Ongoing pain often contributes to depression, anxiety, and sleep disturbances.
- Significantly increases the risk of infertility by reducing egg quality, blocking fallopian tubes, and altering hormonal balance.
- Many patients require assisted reproductive technologies (e.g., IVF) to conceive.
Case Study: A Patient Care Experience
A 32-year-old female patient with a history of five years of painful periods and infertility came with a complaint of pelvic pain and severe. She thought that what she was experiencing was normal pains during menstruation and never sought medical attention early enough. She had vomiting, constipation, bloating and difficulty walking at intervals every month. The painful sex led to emotional distress and her relationship.
Ultrasound showed that she had a 6 cm endometrioma in her left ovary. MRI identified bowel and uterus adhesions. Laparoscopy was stage 4 endometriosis with cysts on both ovaries, and adhesions were dense all over the pelvis. The surgeon excised cysts, separated adhesions and put them back. She was put on hormonal therapy six months after surgery. Pain was also less, bowel movement became normal, and periods became manageable.

Nutrition & Lifestyle Tips
| Item / Activity | Recommended Intake / Duration | Best Time to Take / Perform | Key Nutrients / Benefits |
|---|---|---|---|
| Salmon (Fatty Fish) | 2–3 servings per week (100–120 g per serving) | Lunch or dinner | Omega-3 fatty acids, protein; reduces inflammation |
| Olive Oil (Extra Virgin) | 1–2 tablespoons daily | Use in salads or cooking during lunch/dinner | Healthy monounsaturated fats, antioxidants |
| Nuts & Seeds (Almonds, Walnuts, Chia, Flaxseed) | 1 handful (20–30 g) daily | Morning snack or added to breakfast | Omega-3s, fiber, vitamin E, magnesium |
| Leafy Greens (Spinach, Kale, Swiss Chard) | 1–2 cups daily | Lunch or dinner | Iron, folate, vitamin K, antioxidants |
| Ginger | 1–2 teaspoons fresh or 1 cup ginger tea daily | Morning or after meals | Anti-inflammatory compounds (gingerol), aids digestion |
| Turmeric | ½–1 teaspoon daily with black pepper | Morning with warm water or added to meals | Curcumin (strong anti-inflammatory) |
| Whole Grains (Oats, Brown Rice, Quinoa) | 1–2 servings daily | Breakfast or lunch | Fiber, B-vitamins, sustained energy |
| Water | 8–12 glasses daily | Throughout the day | Hydration, reduces bloating, supports detoxification |
| Avoid: Processed Foods | Completely avoid | — | Reduces inflammation triggers |
| Avoid: Sugar | Completely avoid or limit to < 20 g/day | — | Prevents hormonal fluctuations and inflammation |
| Avoid: Alcohol | Avoid or limit (special occasions only) | Evening (rarely) | Prevents worsening of inflammation |
| Avoid: Caffeine | Limit to 1 cup/day (if tolerated) | Morning | Reduces hormonal imbalance and pelvic pain |
| Avoid: Red Meat | Limit to 1 serving/week or avoid | Lunch/dinner | Lower saturated fats to reduce inflammation |
| Light Yoga | 15–20 minutes daily | Morning or evening | Improves flexibility, reduces pelvic tension |
| Stretching | 10 minutes daily | Morning or pre-bed | Reduces muscle tightness and pain |
| Walking | 20–30 minutes daily | Anytime | Enhances blood circulation, reduces bloating |
| Breathing Exercises | 5–10 minutes daily | Morning or before sleep | Reduces stress hormones (cortisol) |
| Meditation | 10 minutes daily | Morning or evening | Improves emotional stability and reduces pain perception |
When to Seek Medical Help?
Women are to visit a gynaecologist in case they have:
- Severe menstrual pain.
- Suffering in day-to-day life.
- Pain during intercourse or during the passing of faeces.
- Heavy periods with clots.
- More than a year of infertility.
Conclusion
Stage 4 endometriosis is a complicated disorder that leads to intense pain, infertility and organ complications. It is a highly complex disease that can be treated, including surgery, hormonal therapy, pain management, and lifestyle changes. The main key to the prevention of long-term damage is awareness. Women should realise that painful periods are not normal. In case of symptoms, consult a specialist.
Through the appropriate medical attention, emotional support, and good habits, women having stage 4 endometriosis can experience a normative control of their lives, lessen pain and increase their fertility rate.
FAQ‘s
1. What is Stage 4 endometriosis?
The fourth stage is the most progressive stage of endometriosis, where in the disease has proliferated significantly, resulting in huge ovarian cysts, thick scarring and adhesions in the area between organs such as the uterus, ovaries, bowel and bladder. At this stage, pain and infertility are normally extreme.
2. Is it possible to cure Stage 4 endometriosis?
It has no permanent cure, but the symptoms can be well managed. Treatment options include:
- Laparoscopic cyst and adhesion removal.
- Hormonal therapy
- Pain management
- Lifestyle and diet changes
3. Is Stage 4 infertile due to endometriosis?
Yes, it is capable of making people infertile since elements of scar tissue block fallopian tubes, disrupt ovulation processes and distort the placement of pelvic organs. Nevertheless, a large number of women still deliver naturally or through fertility treatment as IUI or IVF, particularly following surgery.
4. What is the method of diagnosis of Stage 4 endometriosis?
Stage 4 endometriosis can be best diagnosed by laparoscopy, which is a less invasive procedure that enables the doctor to peek inside the pelvis and remove lesions as well as take a biopsy. Ultrasound and MRI are used to detect cysts and deep implants.
5. What are the treatment alternatives?
Common treatments include:
- Excision laparoscopic surgery.
- Hormonal drugs (pills, injections, IUD)
- Pain management therapies
6. Does the stage 4 endometriosis recur after surgery?
Well, it can be recurrent as endometriosis is a long-term disorder. Follow-ups, hormonal therapy, an anti-inflammatory diet and an active lifestyle would be useful to minimise flare-ups and enhance long-term outcomes.

 Medically reviewed by
Medically reviewed by