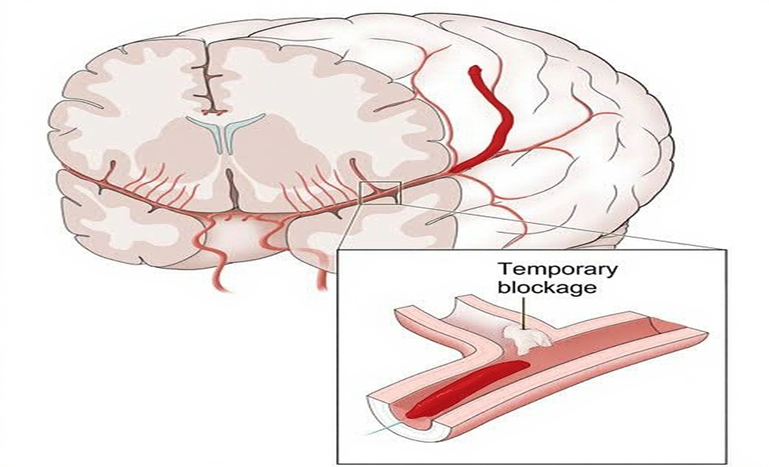
A Transient Ischemic Attack (TIA), or mini stroke, is a temporary episode of neurological dysfunction caused by a brief blockage of blood flow to the brain. TIAs typically last less than five minutes and, unlike a full stroke, do not cause permanent brain tissue damage.
Even a short interruption in blood flow can reduce brain oxygenation and disrupt neuronal perfusion, leading to sudden weakness, speech difficulty, or vision loss symptoms that resolve once circulation is restored.
Difference Between Transient Ischemic Attack and Ischemic Stroke
Both conditions involve reduced blood flow to the brain, a Transient Ischemic Attack (TIA) and an Ischemic stroke differ in duration, tissue damage, and long-term outcomes.
| Feature | Transient Ischemic Attack (TIA) | Ischemic Stroke |
| Nature | Brief interruption of blood supply to the brain, spinal cord, or retina | Prolonged blockage causing infarction (cell death) |
| Brain Damage | No permanent injury | Permanent brain tissue damage |
| Duration | Usually a few minutes; often <1 hour (up to 24 hours in rare cases) | Persistent; symptoms last longer and may be lifelong |
| Imaging Findings | No infarction on CT/MRI | Infarction visible on imaging |
| Risk Implication | Strong warning sign many progress to ischemic stroke soon after | Represents actual brain injury and functional loss |
Causes and Risk Factors of TIA
The roots of a TIA often lie in the cardiovascular system. Understanding these underlying causes is key to both prevention and recovery.
- Atherosclerosis and Blood Clots: A buildup of fatty deposits, known as plaques, in the arteries that supply blood to the brain can narrow these vessels. This narrowing may lead to the formation of blood clots or allow clots from the heart or larger vessels to travel to the brain, temporarily blocking blood flow and triggering a transient ischemic attack (TIA).
- Heart Conditions (Atrial Fibrillation, Valve Disease):Conditions such as Atrial Fibrillation, which causes an irregular heartbeat, can lead to the formation of clots in the heart. These clots can then move into the brain’s circulation, resulting in temporary blockages.
- High Blood Pressure and Diabetes: Both high blood pressure (hypertension) and diabetes contribute to the damage and narrowing of arteries, which increases the risk of experiencing a TIA.
- Lifestyle Triggers — Smoking, Stress, and Poor Diet: Modifiable factors such as smoking, an unhealthy diet, stress, obesity, and a lack of physical activity can increase the likelihood of a TIA by promoting vascular damage and the formation of clots.
Signs and Symptoms
Symptoms generally last a few minutes to less than an hour, with full recovery afterward. Nearly one in three individuals who have a TIA will suffer a Stroke within months if left untreated.
Common warning signs include:
- Weakness, numbness, or paralysis on one side of the face, arm, or leg
- Difficulty speaking or understanding language (dysarthria or dysphasia)
- Blurred or double vision
- Sudden dizziness, loss of balance, or coordination problems
- Confusion, memory difficulties, or behavioral changes
- Headache
Diagnosis
Key Steps in Diagnosis:
Early clinical review:
Healthcare provider or doctor reviews medical history, symptom onset, duration, fluctuations, and may interview witnesses or family members.
Physical and Neurological Exams:
Check strength, reflexes, sensation, coordination, gait, speech, and mental status. Stethoscope is used to listen to carotid artery in the neck for bruit; ophthalmoscope can detect cholesterol fragments, platelet fragments, or emboli in the retina.
Blood Tests:
Measure blood pressure, high cholesterol, diabetes markers, amino acids, and homocysteine to identify risk factors. Aspirin may be given to prevent stroke if no medical reason prevents it.
Imaging and Specialized Tests
- CT and CTA: Computed tomography and angiography create 3D images of the brain and arteries to detect blockages or brain bleed.
- MRI and MRA: Use magnetic field and radio waves to view brain function and cerebral vessels in detail.
- Ultrasound: Carotid duplex ultrasonography or carotid ultrasonography assesses neck arteries; transducer sends sound waves to generate ultrasound images.
- Arteriography: Radiologist inserts catheter via groin incision and injects dye to see cerebral vessels clearly.
Cardiac and Neurological Evaluations
- Echocardiography (TTE or TEE): Detect cardiac sources like mural thrombus or patent foramen ovale causing blood clots.
- Cardiac Monitoring: Telemetry and Holter identifies arrhythmias such as atrial fibrillation, which increase stroke risk.
- Neurological Scales: NIH Stroke Scale, EEG, and other neurological examinations help rule out TIA mimics like seizure, migraine aura, or hypoglycemia.
Treatment Strategies
Medications to Prevent Stroke
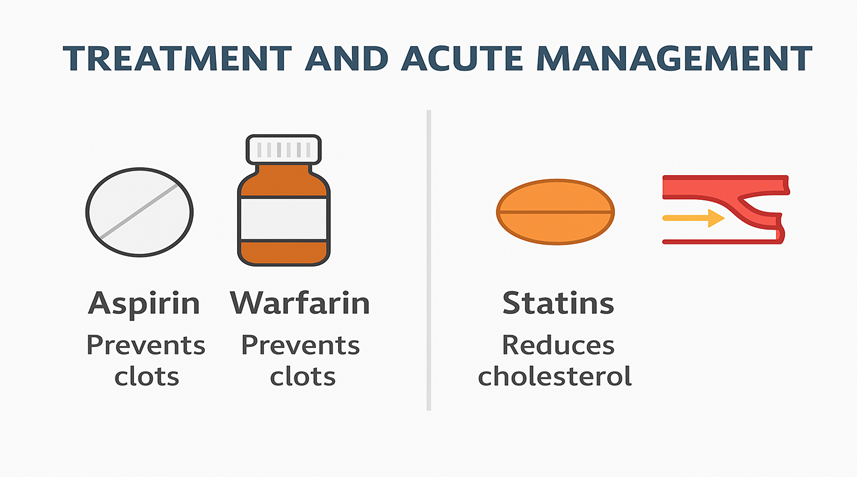
- Anti-platelet drugs like aspirin, clopidogrel, or Plavix prevent platelets from sticking together, reducing clotting in blood plasma. Sometimes, a combination like aspirin plus dipyridamole is used.
- Anticoagulants including heparin, warfarin (Jantoven), or direct oral anticoagulants such as apixaban (Eliquis), rivaroxaban (Xarelto), edoxaban (Savaysa), and dabigatran (Pradaxa) help manage atrial fibrillation and prevent cardiac sources of intracardiac thrombus.
- Dual antiplatelet therapy or single-agent therapy is selected depending on whether the TIA is noncardioembolic or cardioembolic, and dosing may be adjusted according to INR target, mechanical prosthetic valves, or left ventricular thrombus risk.
Surgical and Minimally Invasive Options
- Carotid endarterectomy clears plaques from the carotid artery through an incision and prevents future stroke.
- Angioplasty and stenting involve inserting a balloon device or stent into a blocked artery to restore flow. These minimally invasive endovascular interventions are guided by neurology, cardiology, vascular surgery, or neurosurgery teams.
- In selected patients, patent foramen ovale closure or other revascularization procedures may be recommended to reduce recurrence risk.
Hospital and Monitoring Measures
- Immediate transport to a hospital or emergency department is critical. Rapid initial evaluation, including vital signs, fingerstick glucose, IV access, cardiac monitoring, and pulse oximetry, helps stabilize the patient.
- Laboratory tests like complete blood count, serum electrolytes, coagulation studies, and 12-lead ECG inform therapeutic decisions. Brain imaging via MRI, diffusion-weighted imaging, non-contrast CT, CTA, MRA, or carotid Doppler confirms cerebrovascular status.
- Depending on risk factors and severity, short-term prevention includes antithrombotic therapy, while long-term risk-factor modification focuses on blood pressure, lipids, statin therapy, glycemic control, lifestyle, smoking cessation, alcohol moderation, weight loss, physical activity, diet, and sleep apnea management.
Rehabilitation and Secondary Prevention
Managing Cardiovascular Risk Factors
The American Heart Association emphasizes that maintaining blood pressure, cholesterol, and blood sugar levels within normal limits is essential for vascular health. High blood pressure is the leading risk factor for both TIA and ischemic stroke, as it weakens and narrows the arteries, making them susceptible to blockage or rupture.
- Regularly monitor your blood pressure and aim for readings below 130/80 mm Hg if possible.
- Manage diabetes with appropriate medication and consistent glucose monitoring.
- Treat high cholesterol with statins or other lipid-lowering medications to prevent plaque buildup in blood vessels.
Healthy Living and Regular Screening
- Aim to exercise for at least 150 minutes each week to improve circulation and cardiovascular endurance.
- Adopt a heart-friendly eating pattern that includes plenty of fruits, vegetables, whole grains, and lean sources of protein.
- Avoid tobacco and limit alcohol consumption smoking damages the lining of the arteries, while excessive alcohol intake can raise blood pressure and trigger atrial fibrillation.
- Schedule regular check-ups and screenings for heart rhythm disorders, carotid artery disease, and other vascular issues.
Medication Adherence and Blood Pressure Control
- Antiplatelet agents like aspirin or clopidogrel reduce the chance of clot formation.
- Anticoagulants (for conditions such as atrial fibrillation) prevent dangerous emboli from traveling to the brain.
- Blood pressure control medications help reduce strain on blood vessels and improve overall cerebrovascular health.
A Survivor’s Story
When Dawn Turnage first experienced a transient ischemic attack, she didn’t realize what was happening. The fatigue and dizziness felt like just another stressful day until her words started slurring and her arm went numb. Thinking it would pass, she waited hours before getting help. By the time doctors confirmed it was a “mini-stroke” (TIA), they warned her that she had narrowly avoided a full ischemic stroke. Today, she uses her story to remind others that “time is brain” every minute of delay can mean more brain cells lost.
Her recovery involved not just medication and therapy, but learning to manage her blood pressure, cholesterol, and stress. She now advocates for early checkups and heart-healthy living, showing that surviving a TIA isn’t just about quick treatment it’s about long-term prevention and awareness.
Why Early Recognition Saves Lives?
The NHS “Act FAST” campaign emphasizes that spotting the signs of stroke or TIA early can save lives. Facial drooping, Arm weakness, Speech difficulty, and Time to call emergency services this simple FAST test empowers anyone to respond immediately. Experts note that acting within minutes can restore blood flow before permanent damage occurs.
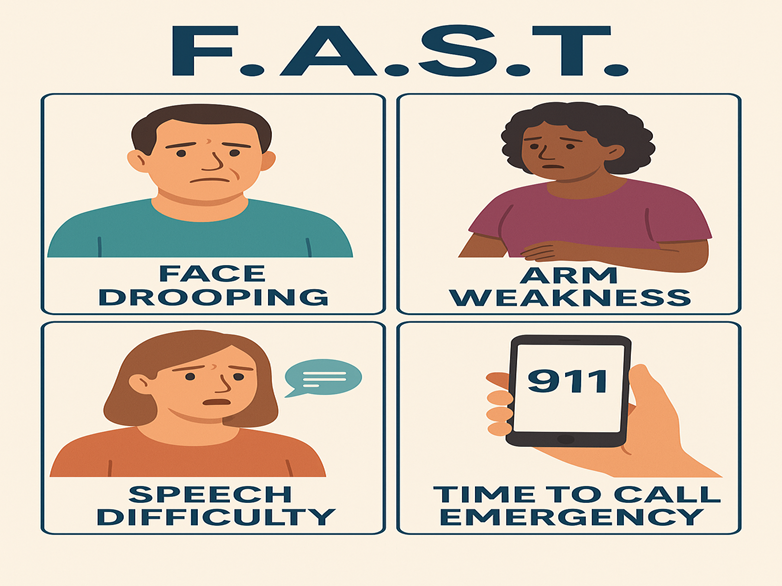
Public awareness remains the strongest defense against long-term disability. Recognizing sudden weakness, slurred speech, or loss of balance even if symptoms last only a few minutes is reason enough to seek emergency care. The message is simple but lifesaving: don’t ignore the warning; act fast and protect your brain.
Conclusion
A Transient Ischemic Attack (TIA) may be temporary, but its message is permanent your body is warning you that your brain and heart need attention. In my public health experience, I’ve seen how recognizing this early can completely change a person’s future. While the episode may last only a few minutes, the window for prevention and recovery begins the moment it happens. Each TIA offers a chance to stop a potentially life-threatening ischemic stroke before it occurs.

 Medically reviewed by
Medically reviewed by