Endometriosis is a chronic gynaecological disorder where endometrial-like tissue proliferates outside the uterine cavity. These ectopic implantations of the endometrium are usually located on the ovaries, pelvic peritoneum and fallopian tubes, and other pelvic organs. It is progressive in nature, and is categorised into four different stages according to the extent of lesions, their depth, and location, in addition to the adhesions, and they are Stage 1 (minimal), Stage 2 (mild), Stage 3 (moderate) and Stage 4 (severe). Stage 1 endometriosis will be the least extensive and the earliest form of the disease, but it still has a serious impact on the quality of life, the state of menstruation, and fertility.
What is Stage 1 Endometriosis?
Minimal endometriosis, or stage 1 endometriosis as it is also termed, is the presence of small, superficial lesions/implants of endometrial tissue with minimal or no scar tissue. The lesions are normally superficial and can be in the form of small spots or patches on the surface of the peritoneum or the organs of the pelvis. As compared to the advanced stages, Stage 1 endometriosis is normally not accompanied by deep infiltrating lesions and widespread adhesions.
Although Terminal 1 of endometriosis is defined as minimal according to surgical results, the level of symptoms manifested in people with Stage 1 endometriosis may be very different and not necessarily correspond to the disease stage.
Aetiology and Predisposing Factors of Stage 1 Endometriosis
The precise nature of endometriosis, even Stage 1 disease, is still not known. Several theories have been postulated, such as retrograde menstruation, in which the ovarian blood flows in a retrograde manner through the fallopian tube and into the pelvic cavity, in which the implantation and growth of endometrial cells occurs. Genetic predispositions also contribute to this since persons who have a family history of endometriosis are more likely to be infected.
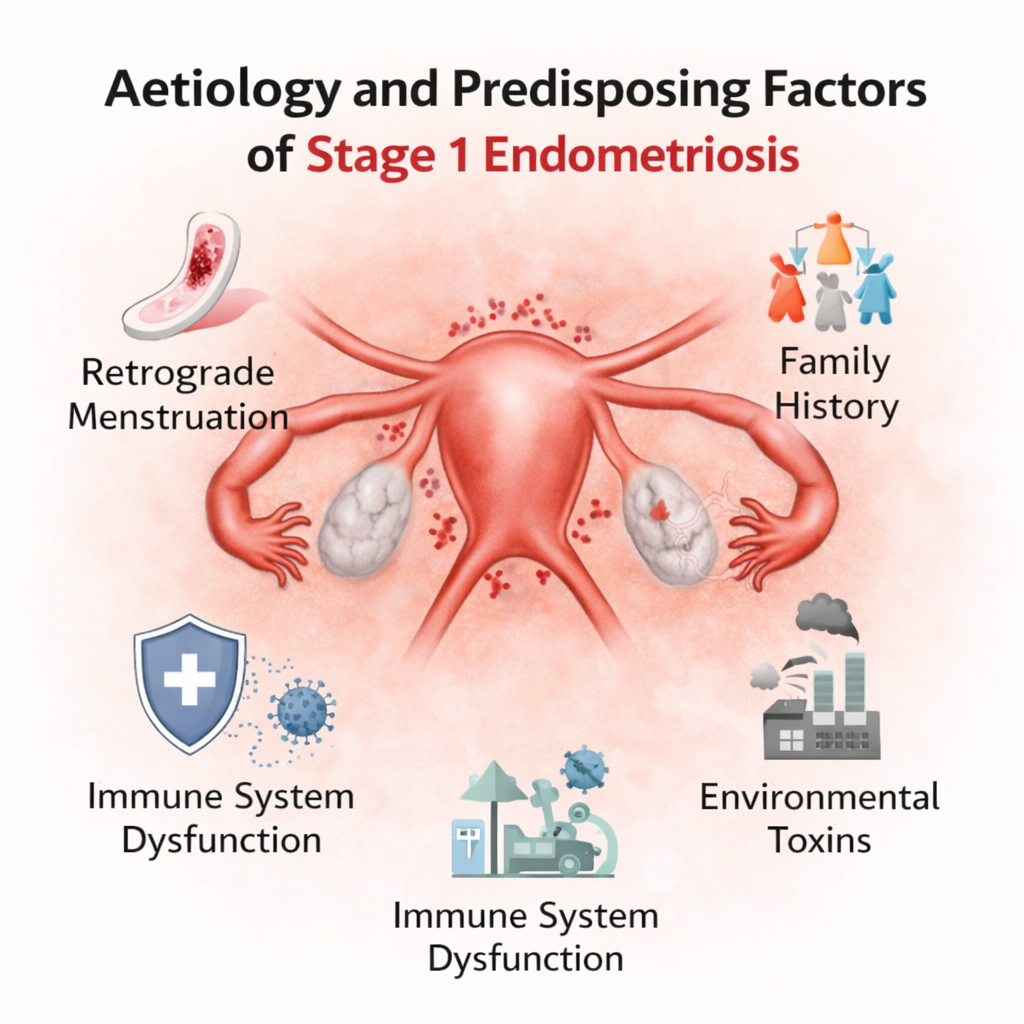
Other factors include hormonal imbalance, especially the predominance of estrogen, dysfunction of the immune system and inflammation. An early onset of menarche, a short cycle, excessive bleeding during menstruation and low body mass index have also been linked to a higher risk of minimal endometriosis.
Symptoms
The lack of correlation between the level of disease and the severity of symptoms is one of the most problematic factors of Stage 1 endometriosis. There are those people with mild endometriosis who are asymptomatic, and there are those who have severe pain and discomfort. They are usually confused with normal menstrual pain, and hence, they are not diagnosed on time.
- Dysmenorrhea, or painful periods
- Chronic pelvic pain
- Lower back pain
- Pain during ovulation
- Dyspareunia or pain during sexual intercourse
- Fatigue
- Bloating
- Nausea
- Gastrointestinal discomfort like constipation or diarrhoea, especially during menstruation
Symptoms such as dysmenorrhea, or painful periods, are common and can only be intensified over time. Even at the early stages of the disease, dyspareunia or pain during sexual intercourse may be experienced.
Stage 1 Endometriosis and Menstrual Health
Even though a minimal form of the disease is considered, Stage 1 endometriosis may have a great influence on menstrual health. Menstrual bleeding may be heavy, prolonged or irregular. The uterine cramping and pain may occur due to the production of prostaglandins caused by the inflammatory environment that is produced by ectopic endometrial tissue. The symptoms can also be worsened by hormonal changes in the menstrual cycle. In the long-term, uncontrolled menstrual pain may disrupt normal life, school, and work performance, hence the need for early diagnosis and treatment of minimal endometriosis.
Fertility Effect of Stage 1 Endometriosis
Stage 1 endometriosis is associated with fertility issues in patients. Even though it is most likely that minimal endometriosis does not cause any structural damage to the reproductive organs, it may subtly lead to fertility issues. A change in the quality of eggs, sperm activity or implantation of embryos may be inflammatory in the pelvic environment.
Early-stage endometriosis can also perturb ovulation and reproductive processes, which is caused by altered immune responses and hormonal imbalances. Although most of the patients with Stage 1 endometriosis indeed have normal deliveries, diagnosis and proper management at an early age are essential for people who are facing the problem of fertility.
Diagnosis
Stage 1 lesions and nonspecific symptoms in the diagnosis of endometriosis may be especially difficult to discover. The first steps should be a comprehensive medical history and pelvic examination, but physical exams are frequent findings are normal in minimal disease. Other imaging modalities (ultrasound and MRI) can be used to exclude other conditions, but lack sensitivity in identifying small superficial implants.
Endometrial lesions can be directly seen and biopsied with laparoscopy, which is the gold standard of diagnosis. In laparoscopic surgery, the presence of minimal endometriosis is a small red, black, or white lesion scattered over the surfaces of the pelvis, which proves the diagnosis and stage.
Surgical Treatment and Its Application
Role of Surgery in Early-Stage Endometriosis
Stage 1 endometriosis may not require surgical intervention when symptoms are mild and can be effectively managed with medical treatment. First-line management typically focuses on symptom control rather than lesion removal, as early-stage disease often involves minimal and superficial implants. Surgery is usually reserved for patients whose symptoms significantly impair daily functioning or fail to improve with conservative therapy.
Indications and Surgical Approaches
Diagnostic laparoscopy is considered in individuals with persistent pelvic pain, severe dysmenorrhea, or infertility despite adequate medical management. This minimally invasive procedure allows direct visualization of endometriotic lesions and enables treatment through excision or ablation. Removal of superficial implants can reduce inflammatory activity, improve pain symptoms, and in some cases enhance fertility outcomes. The choice of surgical technique depends on lesion depth, location, and the surgeon’s clinical judgment.
Medical Treatment and Postoperative Care
Medical treatment remains a cornerstone in the management of Stage 1 endometriosis, both as primary therapy and following surgery. Common options include nonsteroidal anti-inflammatory drugs for pain relief and hormonal therapies such as combined oral contraceptives, progestins, or gonadotropin releasing hormone analogues to suppress disease activity. Because endometriosis can recur, long-term disease control relies on continued medical therapy combined with lifestyle modifications, including regular exercise, dietary adjustments, and stress reduction, to maintain symptom relief and improve overall quality of life.
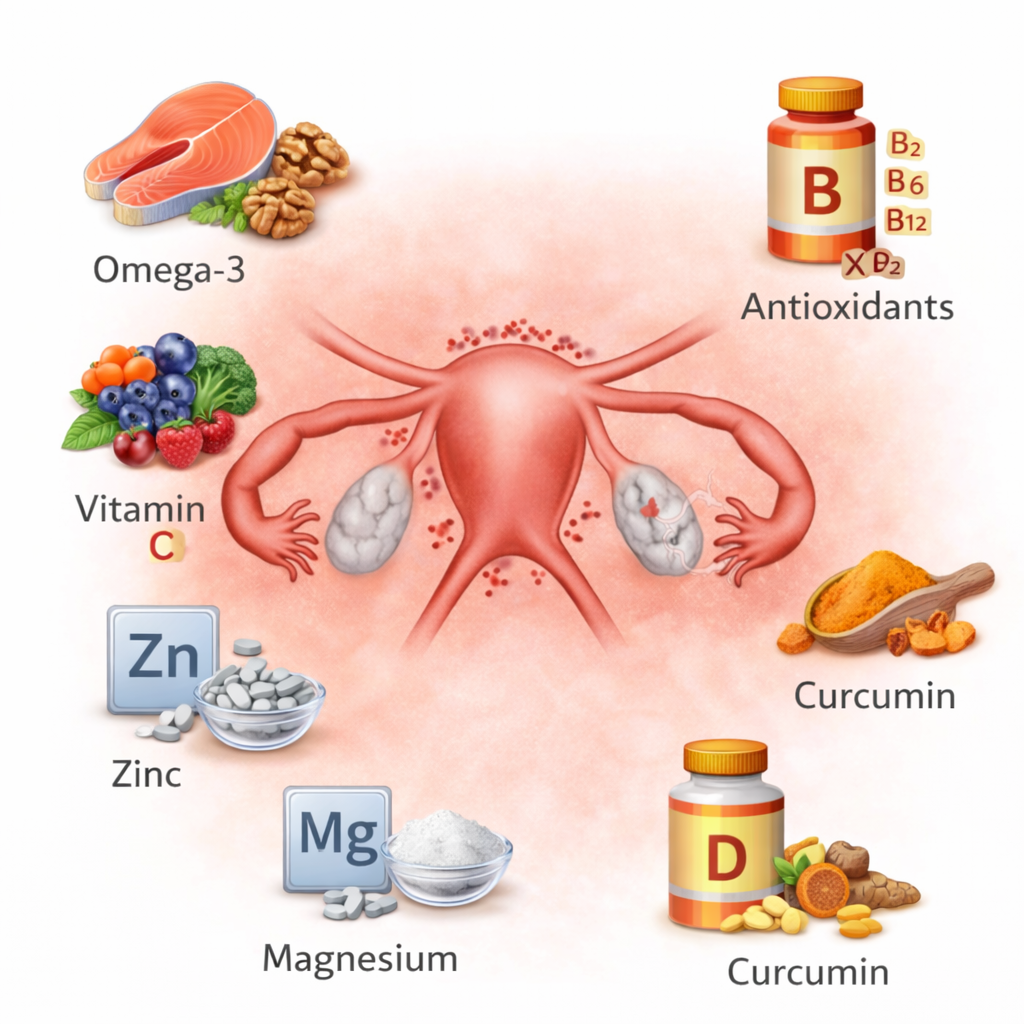
Required Nutrients
| Required Nutrient / Focus | Food Sources (Names) | Recommended Intake Quantity | Practical Portion Quantity |
|---|---|---|---|
| Whole grains | Brown rice, oats, quinoa, whole-wheat bread | 2–3 servings per day | 1 cup cooked grains or 1 slice whole-grain bread per serving |
| Fruits | Berries, apples, oranges, bananas | 2–3 servings per day | 1 medium fruit or ½ cup chopped fruit |
| Vegetables | Leafy greens, broccoli, carrots, bell peppers | 3–5 servings per day | 1 cup raw or ½ cup cooked vegetables |
| Omega-3 fatty acids | Fatty fish (salmon, sardines), flaxseeds, walnuts | 2–3 servings per week (fish) or daily plant sources | 100–120 g fish or 1 tablespoon seeds/nuts |
| Lean protein | Skinless chicken, fish, eggs, legumes, tofu | 1–2 servings per meal | 90–120 g cooked protein or ½–1 cup legumes |
| Gut-supporting foods | Yogurt, kefir, fermented vegetables | 1 serving per day | 1 cup yogurt/kefir or ½ cup fermented foods |
| Micronutrient-rich foods | Nuts, seeds, leafy greens, fruits | Daily inclusion | Small handful nuts/seeds or mixed vegetables |
| Healthy weight support | Balanced meals with controlled portions | Consistent daily intake | Plate method: ½ vegetables, ¼ protein, ¼ whole grains |
| Foods to limit | Processed foods, trans fats, excess caffeine | Occasional or minimal intake | Avoid packaged snacks; limit caffeine to 1 cup/day |
Psychological and Emotional Effects
Emotional Impact and Mental Well-Being
Early-stage endometriosis can affect emotional health despite the limited extent of the disease. Ongoing pelvic pain, painful periods, and other recurring symptoms may lead to frustration, anxiety, and emotional distress, especially when symptoms are misinterpreted as normal menstrual discomfort. Delayed diagnosis and uncertainty about the condition often contribute to feelings of helplessness, low mood, and increased stress levels.
Social, Relationship, and Quality of Life Effects
The physical symptoms of Stage 1 endometriosis can interfere with daily routines, work performance, and social activities, reducing overall quality of life. Pain during sexual intercourse may strain intimate relationships and negatively affect self-esteem.
Concerns about disease progression, future fertility, and long-term management can further intensify emotional strain. Early psychological support, patient education, and stress-reduction strategies are important to help individuals manage both the emotional and social challenges associated with the condition.
Prognosis and Long-Term Outlook
Stage 1 endometriosis has a good prognosis, especially in cases where the disease is diagnosed in time and proper measures are put in place. Medical therapy and lifestyle changes help many people to have good levels of symptom control. The development of the disease is not mandatory, and some individuals can never develop further than mild endometriosis. Close follow-up, periodic monitoring of symptoms, and custom-made changes in treatment are the crucial elements that will help to ensure the long-term health and avert complications.
Conclusion
Stage 1 endometriosis is minimal in nature but a serious health issue which may cause immense impacts on the health of menstruation and fertility, in addition to the quality of life. The initial phase of the disease is an important window of opportunity to diagnose the disease early enough, manage the symptoms and prevent the disease. With the help of medical therapy, lifestyle changes, and emotional care, patients with Stage 1 endometriosis will be able to improve their health results and minimise the cumulative effects of this chronic disease.
FAQ’s
What is Stage 1 endometriosis?
The first type of endometriosis is stage 1 endometriosis or minimal endometriosis. It is also typified by small endometrial implants that are shallow with minimal or no scar tissue. Such lesions typically occur on the organs of the pelvis or on the surface of the peritoneum and do not have deep penetrations or widespread adhesions.
Is Stage 1 endometriosis a cause of severe pain?
Yes, the Stage 1 endometriosis may be a source of considerable pain, even though it is minimal. The level of pain is not necessarily associated with the disease stage. Others get serious menstrual cramps, pelvic pains or pain during intercourse, and others either do not have symptoms at all or have minimal ones.
Can Stage 1 endometriosis be cured?
Endometriosis, including Stage 1 endometriosis, has no permanent cure at present. The symptoms, however, are successfully treated using hormonal therapy, the management of pain, lifestyle modification, and, in limited instances, surgery. Early diagnosis enhances long-term symptom management and quality of life.
Is Stage 1 endometriosis chronic?
Endometriosis is a chronic disease, though possible alterations of symptom patterns may occur at a later age. Proper management allows a good quality of life in many patients with Stage 1 endometriosis, who will have long periods of symptom-free periods.

 Medically reviewed by
Medically reviewed by