The Role of Nutrition in the First Trimester
Nutrition during the first trimester plays a vital role in supporting the early development of your baby. During this critical phase weeks 1 to 12 your baby’s major organs begin to form, including the brain, heart, lungs, spinal cord, and other essential systems. Proper first-trimester nutrition can significantly influence your baby’s long-term health and development.
Why First Trimester Nutrition Matters?
Although the physical changes in your body might not be visible yet, your body is undergoing intense internal transformations. Hormonal shifts, the formation of the placenta, and a significant increase in blood volume all demand specific nutrients even if your caloric needs remain relatively stable (only about 0 to 100 additional calories per day).
What matters most at this stage is not the amount of food but the nutritional quality. Choosing nutrient-dense foods ensures that every bite delivers essential vitamins and minerals without excess calories.
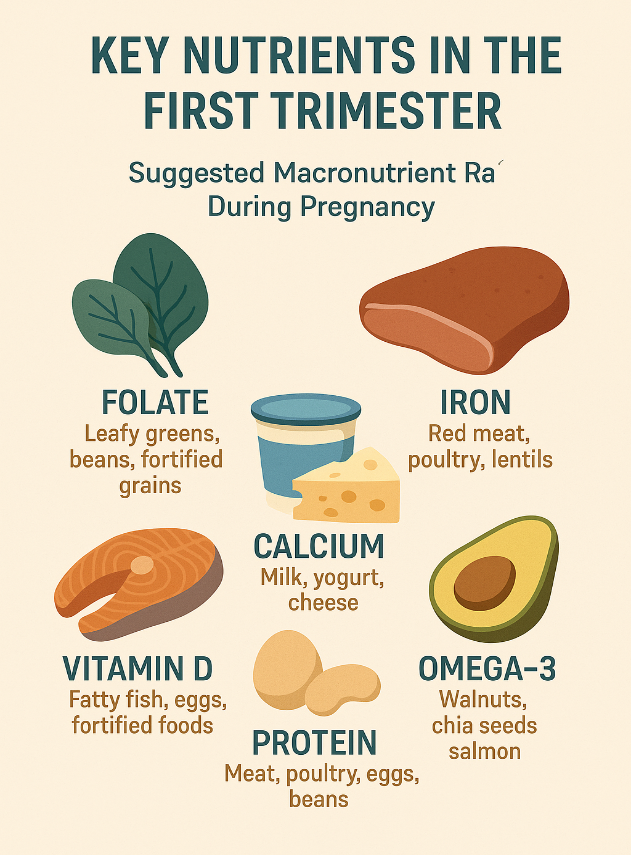
Key Nutrients for the First Trimester
To support healthy fetal development, it’s important to prioritize certain nutrients:
-
Folic Acid (Vitamin B9): Crucial for preventing neural tube defects such as spina bifida. Aim for 400–600 mcg per day through prenatal vitamins and foods like leafy greens, legumes, and fortified cereals.
-
Iron: Supports increased blood production and helps prevent early pregnancy anemia. Iron-rich sources include lean meats, beans, spinach, and iron-fortified grains. Pair with vitamin C for better absorption.
-
Protein: Essential for the development of fetal tissues, including the brain. Good protein sources include eggs, poultry, fish, dairy, tofu, lentils, and nuts.
-
Calcium and Vitamin D: Support bone and dental development. Incorporate dairy, fortified plant-based milk, leafy greens, and safe sun exposure or supplements.
-
Fiber: Helps combat common first-trimester issues like constipation. Focus on whole grains, fruits, vegetables, and legumes.
Best Foods to Eat in the First Trimester
Opt for a balanced and varied diet that includes:
- Whole grains (brown rice, oats, quinoa)
- Fresh fruits and vegetables
- Lean proteins (chicken, turkey, tofu, fish)
- Healthy fats (avocados, nuts, seeds)
- Plenty of water for hydration
Avoid high-mercury fish, unpasteurized dairy, deli meats, and excess caffeine.
Common Misconceptions About “Eating for Two”
You’ve probably heard it before: “You’re eating for two now!” Sounds like a free pass to double up on meals, right? Wrong. This age-old saying is more myth than medical advice especially in the first trimester.
In reality, your baby is about the size of a blueberry by week 7 and doesn’t need much more than what your body is already providing. The phrase “eating for two” has led many expectant mothers to overconsume calories far earlier than necessary, potentially leading to unhealthy weight gain, gestational diabetes, and other complications.
Eating for two means nutrient-sharing, not doubling your portions. You’re feeding both yourself and a developing embryo, so the focus should be on the quality of your food, not quantity. Instead of loading up on extra servings of pasta or dessert, aim for nutrient-rich options that support both your energy and your baby’s growth.
Baseline Caloric Requirements for Women
Factors Affecting Daily Caloric Needs
Before diving into how pregnancy changes your caloric needs, it’s important to understand your pre-pregnancy baseline. Caloric requirements vary wildly from woman to woman based on several personal factors:
- Age: Younger women often have faster metabolisms and may burn more calories at rest.
- Height and Weight: Taller or heavier women may require more calories just to maintain bodily functions.
- Activity Level: If you’re active (say, exercising 4-5 times a week), you’ll naturally need more fuel than someone who’s sedentary.
- Metabolic Rate: Some people burn more calories naturally due to a higher basal metabolic rate (BMR), even when at rest.
Average Caloric Needs Based on Activity Levels
| Activity Level | Caloric Needs (Age 19-30) | Caloric Needs (Age 31-50) |
| Sedentary | 1,800–2,000 | 1,800 |
| Moderately Active | 2,000–2,200 | 2,000 |
| Active | 2,400 | 2,200 |
How Pregnancy Changes Your Metabolism?
Metabolic Adjustments in the First Trimester
Your metabolism starts shifting the moment pregnancy hormones flood your system even before you get that positive test. But these changes aren’t as dramatic in the first trimester as they become later on.
Initially, your basal metabolic rate (BMR) starts to creep up, meaning your body burns slightly more calories at rest. This is largely due to the energy required to support hormonal changes, increased blood production, and the early development of the placenta and fetal organs.
However, the increase in metabolic rate is quite modest during the first trimester. The studies show it rises only about 5-7% above normal. That’s why the increase in calories needed is also relatively small. In most cases, a woman’s body adapts by using existing energy stores more efficiently, rather than demanding a major dietary overhaul.
Interestingly, the body also becomes more insulin-sensitive early on, storing more glucose in preparation for the later trimesters when energy demands spike. It’s like your body is stocking the pantry before the real cooking begins.
Hormonal Shifts and Energy Utilization
Hormones are the unsung heroes (and sometimes villains) of pregnancy. In the first trimester, several hormones impact how your body uses energy:
- HCG (Human Chorionic Gonadotropin): This hormone ramps up quickly and is responsible for most early pregnancy symptoms, including nausea. It doesn’t directly affect metabolism, but it can influence how much you eat or don’t eat.
- Progesterone: It relaxes muscles (including those in your digestive tract), which can slow digestion and cause bloating or constipation. It also helps the body store more fat in preparation for growing the fetus.
- Estrogen: Helps regulate other hormones and plays a part in energy balance, though its direct effect on metabolism is minimal in the first trimester.
First Trimester Caloric Recommendations
Caloric Intake for Normal Weight Women
If you’re starting your pregnancy at a healthy weight, that’s a great foundation. The general rule from most health organizations like the CDC and ACOG is that women of normal weight don’t need to eat any extra calories during the first trimester.
That means if you usually eat around 2,000 calories per day, you can continue doing so. Your body is more than capable of reallocating energy and using its resources efficiently during these first 12 weeks.
However, if you’re experiencing intense fatigue, persistent nausea, or increased hunger, don’t ignore those cues. Listen to your body and aim for nutrient-rich snacks that offer energy without excess sugar or unhealthy fats.
Adjustments for Underweight or Overweight Women
Caloric needs shift a bit if you’re underweight or overweight at the start of your pregnancy.
- Underweight Women (BMI <18.5): You may need to increase your caloric intake slightly even in the first trimester to ensure proper fetal growth. An additional 100–300 calories per day could be beneficial, especially if advised by your healthcare provider.
- Overweight Women (BMI >25): You may not need to increase your caloric intake at all, and in some cases, mild adjustments may even involve slight calorie reduction under medical supervision. The key is to focus on nutrient density, not volume. A smaller quantity of high-quality food can still support a healthy pregnancy.
Ultimately, the goal is gradual, healthy weight gain. The recommended weight gain for the first trimester is just 1 to 4.5 pounds (0.5 to 2 kg).
Macronutrient Distribution for Pregnant Women
In the first trimester, a balanced intake of carbohydrates, proteins, and fats is critical to support both your energy levels and the baby’s early development.
- Carbohydrates are your body’s primary energy source. During pregnancy, they help power everything from cellular activity to organ development. Whole grains, fruits, vegetables, and legumes offer steady energy and fiber, which is especially helpful for managing pregnancy constipation.
- Protein is your building block. In the first trimester, your baby’s tissues and organs begin to form, and protein plays a central role. Foods like eggs, lean meats, beans, and dairy products provide essential amino acids that support growth.
- Fats, especially healthy unsaturated fats, are essential for fetal brain and eye development. Omega-3 fatty acids that is found in fish like salmon and seeds like chia and flax are especially beneficial.
Suggested Macronutrient Ratios During Pregnancy
During the first trimester, general dietary guidelines for macronutrients typically follow this pattern:
- Carbohydrates: 45–65% of total daily calories
- Protein: 15–25% of total daily calories
- Fats: 20–35% of total daily calories
Avoid ultra-processed foods, refined sugars, and trans fats. These offer little nutritional value and can contribute to unhealthy weight gain, inflammation, and blood sugar issues.
Why Hydration Matters More Than Ever?
Water might seem like an afterthought compared to food, but during pregnancy especially in the first trimester hydration is non-negotiable. Every cell, tissue, and organ in your body relies on fluids to function properly, and when you’re pregnant, your fluid needs skyrocket.
Here’s why hydration matters so much in early pregnancy:
- Amniotic fluid production: Water is essential for forming and maintaining amniotic fluid, the cushion that protects your baby throughout pregnancy.
- Increased blood volume: Your body is producing more blood to support the growing placenta and fetus. That extra blood needs fluid to flow smoothly.
- Digestion and nutrient transport: Water helps dissolve and transport nutrients to your baby. It also keeps your digestive system moving, reducing the risk of bloating, constipation, and hemorrhoids.
- Temperature regulation: As your metabolism increases, staying cool becomes harder. Hydration helps regulate your internal temperature, preventing overheating.
But that’s not all. Dehydration in early pregnancy can contribute to fatigue, headaches, and even preterm contractions later on. It can also worsen nausea, leading to a vicious cycle where you feel too sick to drink, but being dehydrated makes you feel even worse.
How Much Water Should You Drink?
So, how much is enough? The general guideline is 8 to 12 cups (64–96 ounces) of fluids per day, but some women need even more depending on activity level, climate, or if they’re vomiting frequently.
Keep in mind, not all fluids are equal. Water is best, but other hydrating options include:
- Herbal teas (like ginger or peppermint)
- Milk (rich in calcium and protein)
- 100% fruit juices (in moderation due to sugar content)
- Broths or soups
- Smoothies
Avoid too many sugary drinks like soda or energy drinks, and limit caffeine to 200mg per day (about one 12-oz coffee) since it can contribute to dehydration in large amounts.
Weight Gain Expectations in the First Trimester
What’s Normal vs What’s Concerning?
One of the most common concerns early in pregnancy is weight gain or the lack thereof. Some women worry they’re gaining too much, while others fear they’re gaining too little. So let’s set the record straight.
In the first trimester, weight gain is usually minimal. Most women gain between 1 to 4.5 pounds (0.5 to 2 kg) during the first 12 weeks. Some women may even lose a little weight due to morning sickness, food aversions, or reduced appetite. That’s generally okay, especially if you were at a healthy weight pre-pregnancy and bounce back in the second trimester.
Pre-Pregnancy BMI
| Pre-Pregnancy BMI | Recommended Total Weight Gain | 1st Trimester Gain |
| Underweight (<18.5) | 28–40 lbs (13–18 kg) | 1–4.5 lbs |
| Normal (18.5–24.9) | 25–35 lbs (11–16 kg) | 1–4.5 lbs |
| Overweight (25–29.9) | 15–25 lbs (7–11 kg) | 0.5–2 lbs |
| Obese (30+) | 11–20 lbs (5–9 kg) | 0.5–1 lb |
Foods to Limit or Avoid Completely
Pregnancy also means some foods are off the table. Certain items carry risks of foodborne illness, high mercury levels, or poor nutrient density.
Here’s what to avoid:
- Unpasteurized dairy or juices
- Raw or undercooked meats and eggs
- High-mercury fish (swordfish, king mackerel, shark)
- Processed deli meats (unless heated to steaming)
- Raw sprouts (risk of E. coli or salmonella)
- Caffeine over 200mg per day
- Alcohol—there’s no known safe amount during pregnancy
And then there are foods to limit, not eliminate:
- Sweets and desserts: okay occasionally, but go easy on sugar
- Fried or greasy foods: can worsen nausea and slow digestion
- Spicy foods: safe, but might irritate your digestive system
Supplements and Prenatal Vitamins
Even with a stellar diet, most pregnant women need a prenatal vitamin. That’s because certain nutrients especially folate and iron are hard to get enough of through food alone.
Here are the must-have nutrients in your first-trimester supplement:
- Folic acid (600 mcg): Prevents neural tube defects
- Iron (27 mg): Supports blood production and oxygen delivery
- Calcium (1,000 mg): Builds baby’s bones and teeth
- Vitamin D (600 IU): Aids calcium absorption and immune function
- Iodine (220 mcg): Supports thyroid and brain development
- Choline (450 mg): Essential for neural development
Managing Cravings and Aversions in the First Trimester
Understanding the Science Behind Cravings
Cravings in pregnancy can feel intense and sudden one minute you’re fine, the next you must have pickles, ice cream, or a weird combo of both. But what causes these cravings in the first trimester, and how should you handle them?
Cravings are often linked to hormonal changes, particularly spikes in estrogen and progesterone. These hormones can alter your sense of taste and smell, sometimes making you more sensitive to certain flavors and triggering emotional or nostalgic food desires. Your body might also be signaling a need for a specific nutrient. For example:
- Craving red meat could point to low iron.
- Craving dairy might mean you need more calcium.
- Craving carbs or sweets might reflect low blood sugar or quick energy needs.
The key is to listen without losing control. Most cravings are harmless in moderation, but it’s easy to overindulge and throw off your caloric balance. The trick is to satisfy your cravings with a healthier twist:
- Want sweets? Try dark chocolate, fruit, or a smoothie.
- Craving crunch? Go for nuts, roasted chickpeas, or carrots with dip.
- Yearning for salt? Opt for sea-salted popcorn or lightly salted edamame.
Coping with Aversions and Sensitivities
Food aversions where certain smells or tastes make you gag are just as common as cravings. In fact, nearly 70% of pregnant women experience strong aversions in the first trimester. These often include:
- Meat, especially red meat or chicken
- Eggs
- Coffee
- Onions or garlic
- Strong cheeses
- Greasy or spicy foods
These aversions are thought to be your body’s way of protecting you from potential toxins, especially during the early, vulnerable stage of pregnancy. But that doesn’t make them any less frustrating especially when they involve nutritious staples like eggs or veggies.
So, what can you do?
- Substitute smartly: If eggs make you queasy, try Greek yogurt or tofu. If meat is the issue, try lentils, beans, or dairy for protein.
- Mask flavors: Try blending disliked foods into smoothies or soups where their taste is less noticeable.
- Cook in batches: The smell of cooking can trigger nausea. Prepare meals ahead of time or ask your partner to help out.
- Eat cold or room temperature foods: These often emit less odor than hot foods, making them easier to tolerate.
Tools and Tips for Monitoring Calories During Pregnancy
Keeping track of what you eat during pregnancy can be helpful but it should never become an obsession. The goal isn’t to restrict yourself, but to ensure you’re meeting your nutritional needs without overdoing it. Here’s how to do that in a healthy, balanced way.
Use a food diary or app: Apps like MyFitnessPal, Ovia Pregnancy, or MyPlate by Livestrong allow you to log your meals and automatically calculate calories and nutrients. These can help you spot deficiencies or patterns (like too few veggies or too much sugar).
Be mindful of portions: You don’t need to weigh every food, but be aware of serving sizes. A “serving” of peanut butter, for example, is 2 tablespoons not half a jar.
Check your energy and hunger cues: If you’re constantly hungry, fatigued, or dizzy, you might not be eating enough. If you feel sluggish or heavy, it could mean you’re overshooting your needs.
Track weight gain weekly: Weigh yourself once a week under the same conditions (e.g., morning, after bathroom, before breakfast). Drastic changes up or down should be discussed with your provider.
Don’t micromanage: Pregnancy isn’t the time for strict dieting or perfect meal planning. Focus on general patterns—are you getting enough fruits, veggies, protein, and water? That’s what matters most.
The Role of Exercise and Activity in Caloric Needs
Exercise and pregnancy? Yes, absolutely. Staying active during the first trimester can help regulate weight gain, boost energy, and improve mood not to mention preparing your body for the demands of labor.
But if you’re moving more, you’re burning more. That means your caloric needs might slightly increase but only slightly. For example:
- A 30-minute brisk walk might burn 120–150 calories.
- A prenatal yoga session might burn 100–200 calories.
- Light strength training could burn 150–250 calories.
So, should you eat back those calories? That depends on your hunger and how you feel. If your workout leaves you feeling depleted, a post-exercise snack with protein and carbs (like a banana with peanut butter or a yogurt parfait) is a great idea.
The first trimester is a time to focus on gentle, consistent movement not intense calorie burning. Safe activities include:
- Walking
- Swimming
- Prenatal yoga
- Stationary biking
- Light weight lifting (with modifications)
Conclusion
The first trimester is a delicate but powerful stage of pregnancy. While the caloric increase isn’t huge typically only 0 to 100 extra calories per day your nutritional needs are more important than ever. Every bite matters, not just in energy, but in what it delivers: folate, iron, calcium, protein, fiber, and healthy fats.
Listen to your body, stay hydrated, manage cravings wisely, and prioritize nutrient-dense foods. Trust that small, consistent choices will build the foundation for a healthy pregnancy and a healthy baby.
FAQs
Do I need to eat extra calories in the first trimester?
Not necessarily. Most women don’t need extra calories during the first 12 weeks unless they’re underweight or very active. Focus on quality over quantity.
Is it okay if I lose weight in the first trimester?
Mild weight loss due to morning sickness is normal. If weight loss is significant or persistent, contact your healthcare provider.
What if I can’t eat healthy because of nausea?
Do your best. Stick to bland, easily digestible foods and focus on hydration. Nutrient-rich snacks and prenatal vitamins can help fill the gap.
Can I exercise during the first trimester?
Yes! Light to moderate exercise like walking, swimming, or yoga is safe for most women and can help manage weight gain and boost mood.
Are cravings a sign that something’s missing in my diet?
Sometimes. Cravings may reflect nutrient needs, but not always. It’s okay to indulge occasionally, but aim to satisfy cravings with healthier versions.

 Medically reviewed by
Medically reviewed by